French pharmaceutical giant Sanofi recently announced that the US Food and Drug Administration (FDA) has approved the single-domain antibody (sdAb) drug Cablivi (caplacizumab) combined with plasma exchange and immunosuppressive therapy, for the treatment of acquired thrombotic thrombocytopenic purpura (aTTP) adult patients with acquired thrombotic thrombocytopenic purpura. The approval makes Cablivi the first drug in the United States to specialize in the treatment of aTTP.
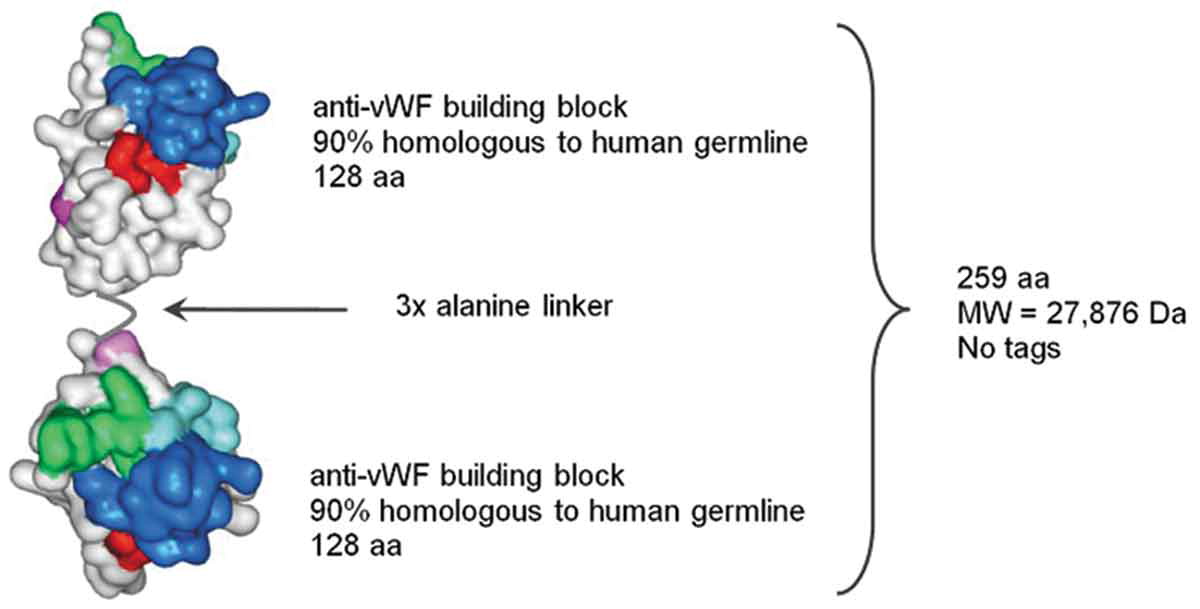
Figure 1. Schematic structure of caplacizumab. (Sargentini-Maier, 2019)
Cablivi was acquired after Sanofi spent $4.8 billion on Belgian biotechnology Ablynx, which was approved by the European Union at the end of August 2018 for adult patients who have experienced an aTTP attack. The approval makes Cablivi the world’s first approved sdAb drug and the first drug specifically designed to treat aTTP. Cablivi has been granted orphan drug qualifications for the treatment of aTTP in the United States and the European Union, as well as fast-track qualifications and priority review qualifications in the United States.
ATTP is a life-threatening, autoimmune-based coagulation disorder characterized by the formation of large amounts of blood clots in small blood vessels throughout the body. Leading to severe thrombocytopenia (extremely low platelet count), microangiopathy, hemolytic anemia (loss of red blood cells due to hemolytic destruction), tissue ischemia (limited blood supply in parts of the body) and extensive organ damage, Especially the brain and heart. Despite current standard care regimens, including daily plasma exchange (PEX) and immunosuppressive therapy, patients still face a high risk of thrombotic complications, recurrence, and death, and aTTP seizures are still associated with up to 20 percent mortality. Most of the deaths occurred within 30 days of diagnosis.
The active drug component of Cablivi is caplacizumab, which is a potent and selective bivalent anti-von Willebrand factor (vWF) sdAb, which can block the interaction between very large vWF polymer (ULvWF) and platelets. It has an immediate effect on platelet aggregation and the subsequent formation and accumulation of small blood clots (microclot). In patients with aTTP, this tiny blood clot can lead to severe thrombocytopenia, tissue ischemia, and organ dysfunction. This transient effect of Cablivi (immediate effect,) can not only dismantle the potential disease process, but also protect the clinical manifestations of aTTP patients.
The approval of Cablivi was based on data from the Phase III Clinical study HERCULES (NCT02553317). The study was a randomized, double-blind, placebo-controlled study of 145 adult patients with aTTP. In the study, patients were randomly assigned to Cablivi or placebo and received standard care regimens (plasma exchange and immunosuppressive therapy).
The results showed that: (1) in terms of the main endpoints, Compared with placebo + standard nursing regimen, Cablivi combined with standard nursing regimen significantly shortened the time to normalize platelet count (p ≤ 0.01); at any particular time point during the study period, the possibility of reaching normal platelet count in Cablivi treatment group was. The placebo group was 1.55 times as much as the placebo group. (2) compared with placebo + standard nursing regimen, Cablivi combined with standard nursing regimen significantly reduced aTTP-related deaths, aTTP recurrence or at least one major thromboembolism event by 74 percent throughout the study period (p < 0.001). (3) during the whole study period, compared with placebo + standard nursing regimen, Cablivi combined with standard nursing regimen significantly reduced the recurrence of aTTP by 67% (p < 0.001). (4) throughout the study period, there were 0 refractory diseases in the Cablivi group and 3 refractory diseases in the placebo group, although there was no significant difference (p ≤ 0.06). (5) compared with the placebo group, the normalization of three organ injury markers (lactate dehydrogenase, cardiac troponin I, serum creatinine) occurred earlier in Cablivi group (p did not detect significant due to stratified statistical test). (6) the use of plasma exchange in Cablivi group was significantly lower than that in the placebo group (mean 5.8 days vs 9.4 days, a decrease of 38%). And stay in intensive care units (a decrease of 65 percent) and hospitals (a decrease of 31 percent) is even shorter. (7) the safety of Cablivi is consistent with previous reports and accords with its mechanism of action, including the increased risk of bleeding; the most common bleeding-related adverse events are epistaxis and gingival bleeding.
Marie Scully, a professor of hematology at the University of London Hospital and lead researcher of the HERCULES study, previously said, “aTTP is a life-threatening disease and the current treatment does not completely prevent widespread thrombosis in small blood vessels throughout the body. This puts patients at risk of serious morbidity and premature death. Our research shows that Cablivi has the potential to address significant unmet medical needs in this area and to help patients facing potentially devastating consequences. “
Reference
1. Sargentini-Maier, Maria Laura, et al. “Clinical pharmacology of caplacizumab for the treatment of patients with acquired thrombotic thrombocytopenic purpura.” Expert review of clinical pharmacology 12.6 (2019): 537-545.
