 In this month, FDA oncologic Drugs Advisory Committee agreed to the approval of Novartis’s CAR-T CTL019 therapy on a vote of 10:0 for the treatment of relapsed or refractory children and young adult B cell acute lymphoblastic leukemia. Such news makes this therapy attracts great attention.
In this month, FDA oncologic Drugs Advisory Committee agreed to the approval of Novartis’s CAR-T CTL019 therapy on a vote of 10:0 for the treatment of relapsed or refractory children and young adult B cell acute lymphoblastic leukemia. Such news makes this therapy attracts great attention.
As a kind of cancer immune therapy, CAR-T therapy has made exciting achievements in the treatment of hematologic malignancies. Emily Whitehead, the world’s first one to accept experimental CAR-T therapy (patient with acute lymphoblastic leukemia), is now 12 years old. She still has not had a relapse after receiving CAR-T therapy for 5 years.
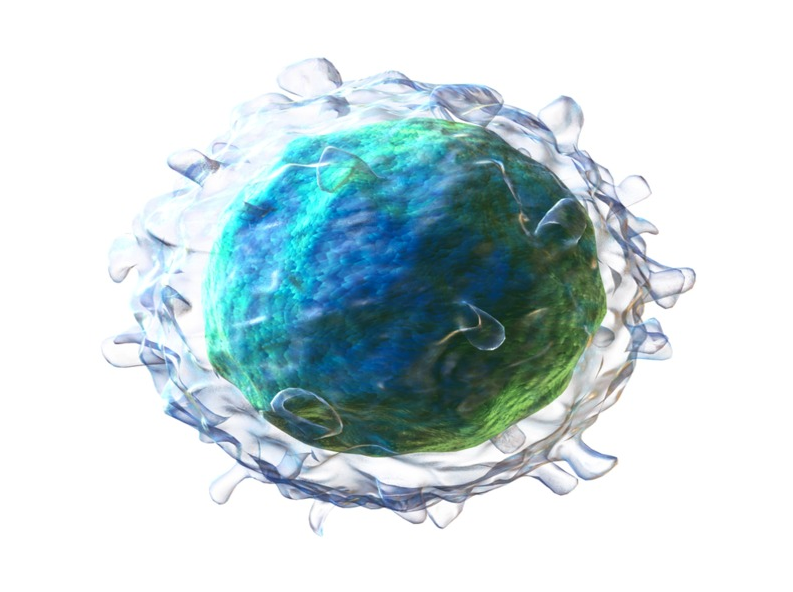
CAR-T is different from the typical small molecules or biological treatment, because it is the therapy to use the patient’s own cells. In simple terms, this kind of therapy isolates the T cells from the patients themselves, and transforms these t cell in vitro by putting a “navigation” to specific recognize cancer cells—chimeric antigen receptor (CAR). After that, the “modified CAR-T cells” are infused back into the patient to play a specific anti-tumor effect.
Professor Carl H. June of the University of Pennsylvania is recognized as a specialist in CAR-T area. The above mentioned CTL019 was first led and developed by him. Recently, we noted that his name appeared in the latest paper published on the Journal of Science Translational Medicine. This paper announced the preliminary results of CAR-T human trials for a solid tumor.
In fact, the use of CAR-T therapy for solid tumors has been the direction of researchers in the field. Although a number of clinical trials are under the way, there is no data to objectively prove that CAR-T is effective against any solid tumors.
The latest research results show that in clinical trials of CAR-T therapy, the modified T cells successfully migrate and penetrate into a deadly brain tumor (glioblastoma, GBM), but these cells trigger the immunosuppressive tumor microenvironment, and face a complex mutation.
New research reveals two major obstacles
In the past two years, researchers from the University of Pennsylvania’s Perelman School of Medicine reported the results of human trials for the treatment of GBM with CAR-T therapy. The CAR-T cells were able to track down and kill cancer cells expressing tumor-specific-protein EGFRvIII. Experiments showed that CART-EGFRvIII cells had acceptable safety, and can cross the blood-brain barrier in tumor that lead to immune response, resulting in EGFRvIII tumor antigen decrease in GBM cells.
The newly published study included all results from 10 patients with initial treatment. The paper revealed two major obstacles in the treatment of GBM: 1. there were wide variations in the expression of EGFRvIII; 2. the emergence of drug resistance in the tumor microenvironment (the researchers found that the immunosuppression of tumor microenvironment became stronger after reinfusion of CAR-T to the patient). The authors say that overcoming the first hurdle may require targeting additional antigens, and the use of existing targeted immunosuppression molecules, such as checkpoint inhibitors, may overcome second hurdles.
Dr. Donald M. O ‘Rourke said: “this is a test in the early stage. Cells can enter the brain to proliferate. So that antigen levels decrease, and little toxicity is for patients. These results have inspired us to carry out further research for the next step”.
Specific trail result analysis
Specifically, in the study, the 10 refractory & recurrent GBM patients received a single CAR-T cell transfusion therapy, which were divided into 3 groups: 1. 3 patients did not receive surgery after CAR-T transfusion; 2. 3 patients accepted the “late surgery” respectively 34 days, 55days and 104 days after infusion of CAR-T; 3. 4 patients, who had the “early surgery” with obvious symptoms of progress, accepted CAR-T transfusion regimen followed by surgical treatment.
In the first two weeks after infusion of CAR-T cells, 4 patients receiving early surgery can be detected numbers of CART-EGFRvIII cells in the tumor, and those cells revealed the signs of activation. In all patients’ blood with CAR-T transfusion, there had been found circulating CART-EGFRvIII cells. However, the level of CART-EGFRvIII cells in the blood began to decline in two weeks. After a month, it could not be detected at all. In addition, the researchers observed that in the tumor of the 5 patient who underwent surgery after CAR-T reinfusion, the level of target antigen EGFRvIII decreased.
At the same time, it was also found that with the passage of time and in different areas of tumor, the expression of EGFRvIII would be extensively mutated. This showed that single target is not enough to gain lasting clinical benefits. Besides, CAR-T therapy could trigger the production of immune suppression regulatory T cells, and these cells would be transferred to tumor, resulting in additional immunosuppressive pathway up-regulation.
The main research of phase I is safety, rather than curative effect, so it cannot identify the clinical benefits of CART-EGFRvIII therapy. However, 1 patient was in stable condition in the 18 months follow-up, and was still alive till his data was published. Another two patients were also alive, and their symptoms appeared in progress. The rest of the 7 patients were living longer than expected.
Finally, back to the safety, CART-EGFRvIII therapy showed acceptable safety in all patients. In the study, there was no sign of cytokine release syndrome which was a serious toxic effect observed in other CAR-T tests. In the experiment, one patient showed epilepsy. But anti-epileptic drugs also successfully controlled this symptom. Although safety was satisfactory, it should be emphasized that in any patient, researchers never observed significant tumor regression through magnetic resonance imaging.
Dr. O’Rourke said:” this is an important paper, because it proves the important potential of CAR-T therapy in glioma therapy. At the same time, the paper also points out the two major problems the current technology facing: antigenic heterogeneity and tumor microenvironment resistance. It will guide us and other researchers in the field to move in the right direction “.
