Swiss pharmaceutical giant Roche recently announced that the Food and Drug Administration (FDA) has accepted the biologics licensing application (BLA) of polatuzumab vedotin, antibody drug conjugate (ADC), and granted priority review. The BLA applied for polatuzumab vedotin combined with bendamustine and Rituxan (meropenem, commonly known as rituximab) for the treatment of patients with recurrent or refractory diffuse large B-cell lymphoma (R/R DLBCL).
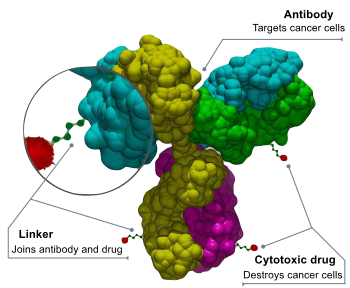
Structure of an antibody-drug conjugate
FDA has set a target date of August 19, 2019 for the Prescription Drug User Fee Act (PDUFA). Previously, polatuzumab vedotin was granted orphan drug designation by FDA and EU EMA, as well as breakthrough therapy designation (BTD) and priority medicine (PRIME), respectively.
Polatuzumab vedotin is a kind of first-in-class, anti-CD79b ADC, and is formed by coupling anti-CD79b antibody with anti-mitogen MMAE (monomethylaspirin E). The highly specific expression of CD79b in most types of B-cell non-Hodgkin’s lymphoma (NHL), is an attractive target for the development of new therapies. Polatuzumab vedotin targets CD79b and destroys these B cells, maximizing the catalysis of cancer cells while minimizing the effect on normal cells.
Polatuzumab vedotin BLA is based on positive data from a randomized phase Ib/II clinical study, GO29365 (NCT02257567). The study was carried out in patients with histologically confirmed R/R follicular lymphoma (FL) or DLBCL. The efficacy and safety of intravenous infusion of polatuzumab vedotin combined with standard dose bendamustine (B) and rituximab (R) three-drug regimen (PBR) were evaluated compared with standard dose bendamustine (B) and rituximab (R) second-drug regimen (BR).
A total of 80 patients with R/R DLBCL who had previously been overpretreated were enrolled in the phase II clinical study and were not eligible for hematopoietic stem cell transplantation. The data showed that compared with the BR two-drug regimen, the PBR three-drug regimen significantly prolonged the overall survival (median OS: 12.4 months vs 4.7 months, HR=0.42, 95%CI: 0.24-0.75; exploratory endpoint). In addition, compared with the BR two-drug regimen, the PBR three-drug regimen also significantly increased the complete remission rate (CR: 40% vs 18%, primary endpoint) and reduced the risk of disease progression or death by 66% (median PFS: 7.6 months vs 2.0months, HR=0.34, 95%CI: 0.20-0.57), prolonging the duration of mitigation (median DOR: 10.3 months vs 4.1 months, HR=0.44).
DLBCL is the most common non-Hodgkin’s lymphoma (NHL), accounting for about 1/3 of NHL cases. DLBCL is an invasive (rapidly proliferating) type of NHL that recurs in up to 40 per cent of patients and has a poor prognosis. It is estimated that more than 22000 new cases of DLBCL will be added in the United States in 2019. If approved, the PBR three-drug regimen will provide an important new treatment option for a significant prolongation of survival in the R/R DLBCL population.