Vascular dysfunction contributes to the pro-oncogenic tumor microenvironment and impedes the delivery of therapeutic drugs, so normalizing tumor blood vessels may become a potential path. Scientists have developed a new type of therapeutic antibody that may dredge and normalize blood vessels in cancerous tumors, thus providing a more effective drug delivery pathway for targeted cancer treatments, according to a study published on bioRxiv.
Chaotic angiogenesis is the main cause of a variety of diseases, including cancer. By studying mice, the researchers demonstrated for the first time that inhibiting the activity of the leucine-rich α-2-glycoprotein 1 (LRG1) might normalize chaotic blood vessels. They said the new drug may lead to better treatment for patients who do not respond well to the current standard treatment for cancer. In addition, the new antibody can significantly enhance the ability of immunotherapy to inhibit the progression of solid tumors, a problem that clinicians and scientists have been trying to solve.
According to Professor John Greenwood, tumor cells need blood vessels to provide nutrients to grow. When new blood vessels are formed inside the tumor, these vessels become abnormal and affect oxygen transport, making the tumor more aggressive. This abnormal vascular supply may limit the delivery of anticancer drugs, reducing their effect and causing cancer cells to develop tolerance. So the researchers wondered whether blocking the activity of the LRG1 protein, which damages blood vessels, could promote normal blood vessel growth, reduce tumor expansion, and enhance the delivery and therapeutic effects of other drugs.
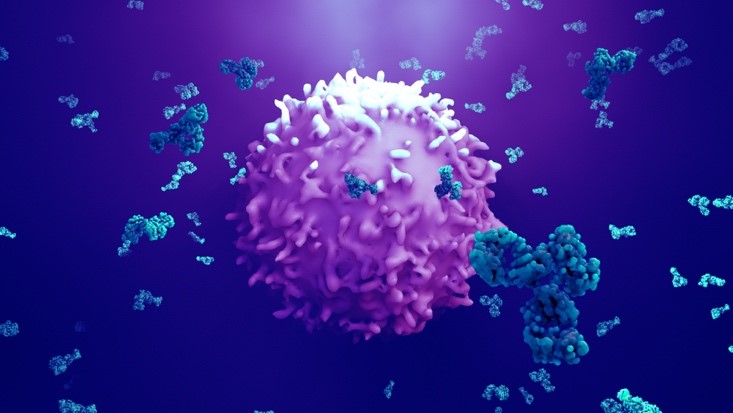
The researchers pointed out that antibodies that block LRG1 can be used in a wide range of cases in mice that carry tumors. In the cancer model studied, when used alone, the antibody could significantly improve blood flow and oxygenation, and reduce the tumor growth rate. When combined with chemotherapy or immunotherapy, there is obviously an increase in immune cell penetration and tumor cell lethality compared with monotherapy.
Professor Stephen Moss believes that finding a way to normalize the blood vessels of cancerous tumors may be a clinical goal, but identifying an effective therapeutic tool has proved to be quite difficult to achieve. The results of this study may provide direct evidence that blocking LRG1 protein may normalize blood vessels and enhance the suboptimal efficacy of immunotherapy in solid tumor therapy, including checkpoint inhibition and CAR-T cell therapy. This may provide new hope for many cancer patients who do not respond well to the current standard care to achieve better therapeutic results.