Introduction
For many years, non-human primates (NHPs) have served as a key biological test bed because they are genetically and physiologically comparable to humans. At Creative Biolabs, we know how important NHP models are for improving the treatment of complex human disorders, including liver disease. In this blog, we look at one recent experiment that used NHPs to simulate acute liver failure (ALF), a highly morbid and fatal condition, and how our NHP biologicals can aid in similar studies.
The Paper: Nonhuman Primate Acute Liver Failure Model
Abstract
The research was entitled “An animal non-human primate model of acute liver failure to investigate liver support systems,” aimed to produce a solid, large animal model of hepatic failure with human-like characteristics. The team induced ALF in NHPs with liver-directed radiation therapy and liver ischemia-reperfusion injury. This not only mimicked the pathophysiology and pathology of clinical ALF but also led to 100% mortality—ideal as a model in which to test liver support or replacement therapies in a preclinical setting.
Background
Acute liver failure (ALF) is a chronic disease where liver failure develops rapidly, leading to multiorgan failure and death. The only permanent cure for ALF is liver transplantation, which has high risks and is in short supply. Creating efficient liver support systems could make a difference for transplant candidates or help people recover from irreversible liver damage. However, the rarity of severe ALF, variability in clinical presentation, and inconsistent results have hindered the development and evaluation of such systems. An animal model of liver failure with a high window of opportunity to test intervention effectiveness and timing is urgently needed.
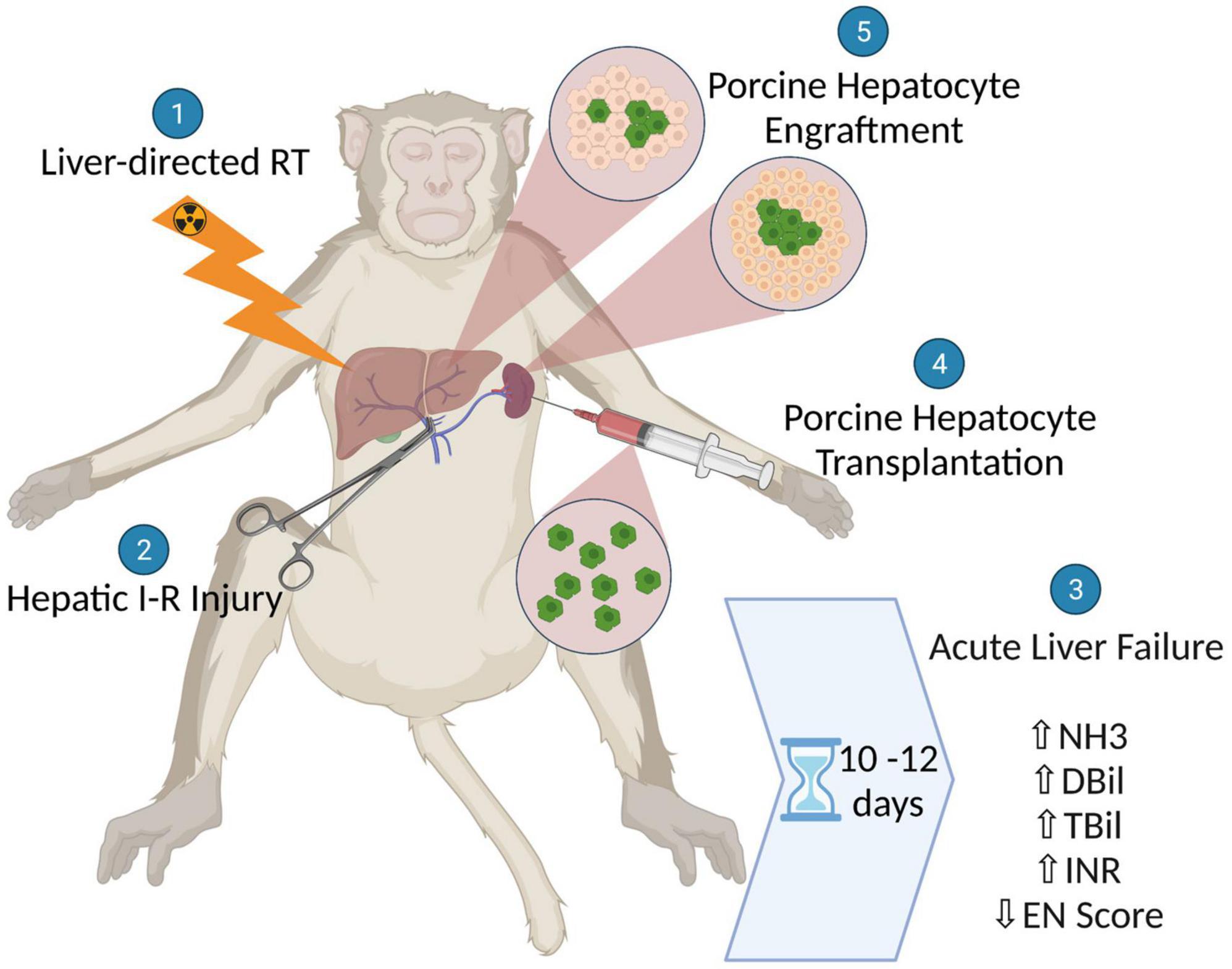
Fig.1 Schematic illustration showing the generation of a non-human primate model for acute liver failure (ALF) using liver-directed radiation therapy followed by hepatic ischemic-reperfusion injury and the subsequent assessment of xenogeneic hepatocyte transplantation as a potential therapy for ALF.1
Methods
The scientists used a two-step process to induce ALF in NHPs. First, the NHPs received liver-directed radiation therapy (RT) to damage and disturb liver regeneration. RT was delivered as a 6MV beam to a CLINAC 23IX Varian accelerator in five fractions of a 35Gy prescribed dose. For positioning, the care used CT scans and cone beam computed radiotherapy (CBCT).
Next, a benign hepatic ischemia-reperfusion (I-R) injury was inflicted to produce fatal ALF. I-R damage was induced by blocking the portal triad (extrahepatic portion of the hepatic portal vein, hepatic artery proper, and common bile duct) for 80-150 minutes. The clamps were released after the ischemia time, and the NHPs were monitored for healing and liver function.
Results
The liver-directed RT and hepatic I-R injury combination successfully and quickly caused ALF in NHPs. The NHPs had severe liver failure, with elevated ammonia, total and direct bilirubin, INR, and encephalopathy scores, and were 100% dead. Histological examination showed necrosis, disappearance of hepatocytes, and parenchymal collapse, typical of acute liver failure. Xenogeneic hepatocyte transplantation as a potential ALF treatment was also tested using this model.
Discussion
This NHP model of ALF represents a significant advancement in hepatology. The model’s potential to induce ALF consistently with predictable kinetics and homogeneous pathophysiology makes it a good candidate for testing new liver support mechanisms and therapies. The results show that xenogeneic hepatocyte transplantation as a treatment option, but there is still more to learn about optimal engraftment and immune suppression regimens.
NHP Biologicals from Creative Biolabs: A Powerful Contribution to Hepatology Research
Creative Biolabs offers NHP biologicals that play an important role in hepatology research, for example, ALF. We create products and services to help scientists stay ahead in their research and develop useful treatments.
1. NHP Cell Lines: Our immortalized NHP cell lines provide a stable and high-quality primate cell source for all sorts of experiments. These cell lines can be used to study the cell processes that drive liver pathologies, evaluate the effectiveness of therapies, and investigate the impact of drugs on liver cells. Scientists can, for instance, use these cell lines to examine the effects of radiation and ischemia-reperfusion damage on hepatocyte function and survival.
2. NHP Plasma and Serum: Our NHP plasma and serum products are essential in biomedical research in immunology, virology, neuroscience, and metabolism. They can be applied to study the immune response in ALF, the metabolic mechanisms of liver failure, and the creation of diagnostic markers for liver disease. In the ALF model, NHP plasma could also be used to track systemic inflammatory and metabolic disruptions during liver failure.
3. Modified NHP Models: We know every research project is unique. Our NHP model design service enables researchers to build and run NHP models tailored to their specific research challenges. We are the team to help bring your research to life, whether it involves inducing certain liver damage or experimenting with new liver support devices. For example, we can support researchers who want to develop models with different ischemia times or different radiation doses to investigate the dose response to ALF.
4. Quality Control & Assurance: Creative Biolabs is all about quality and stability of the product. We do everything we can to ensure that our NHP biologicals pass our quality control and researchers can trust their experiments. This is especially true in research on complicated treatments such as radiation therapy and cell transplantation, for which the quality of biological material could make all the difference.
Why NHP Models Are Crucial to Hepatology?
Having constructed the NHP model for ALF, we have shown that NHPs are instrumental in the progress we make in liver disease. NHPs also afford a chance to investigate the liver’s intricate interplay with other organs, the immune response to liver failure, and regenerative medicine in general. In addition, NHP models could help us jump-start the process between in vitro research and clinical trials to make valuable decisions about whether or not new treatments are safe and effective.
Linking In Vitro and In Vivo Research
There is no good in vivo model of human disease that can match up to the lab. NHP models like the one here create an important intermediary by offering a physiologically valid system for hypothesis testing and treatment evaluation. By triggering ALF in NHPs with known kinetics, it is possible to monitor disease progression in near real-time and test the effects of interventions under a microscope.
Advancing Regenerative Medicine
Regenerative medicine is a promising field for treating liver diseases. The ALF NHP model allows us to explore cell-based therapies (such as hepatocyte transplantation) to regenerate livers. Testing these treatments in NHPs could help scientists understand the engraftment, survival, and function of transplanted cells and inform the design of trials in humans.
Learning About Immune Responses to Liver Failure.
ALF is pathophysiologically influenced by the immune system. In NHP models, researchers can test how complex immune responses—such as the activation of innate and adaptive immunity, cytokine production, and immune cell-hepatocyte communication—unfold in liver failure. This information can be used to build immunomodulatory drugs that suppress the inflammatory response and help patients.
Conclusion
Acute liver failure in NHPs is a big step in hepatology. With a predictable and replicable model of ALF in hand, scientists can now test a variety of therapies and interventions in a laboratory-like setting. Creative Biolabs stands ready to contribute to this research with our full line of NHP biologicals. We expect our NHP models and biologicals to help solve the mysteries of liver disease and create life-saving therapies. Whether it’s analyzing cell processes, discovering diagnostic markers, or conducting clinical trials of novel therapies, Creative Biolabs will partner with the scientific community to improve human health.
Future Directions
This NHP model of ALF opens up new research and therapeutic possibilities. The next step could be improving the model to better resemble human conditions, testing combinatorial treatments, and exploring the long-term effects. It may also be possible to use the model to study the molecular and cellular mechanisms involved in liver regeneration and fibrosis, two key stages of liver disease progression and repair.
Reference:
- Kalsi RS, Ostrowska A, Olson A, Quader M, et al. A non-human primate model of acute liver failure suitable for testing liver support systems. Med.2022. 9:964448.
- Distributed under Open Access license CC BY 4.0, without modification.
