Hepatocellular carcinoma (HCC) is the most common form of primary liver cancer and the leading cause of cancer-related deaths worldwide. Despite advances in the treatment of advanced hepatocellular carcinoma in recent years, its 5-year survival rate is still less than 10%. Advanced hepatocellular carcinoma is a relatively immunotolerant tumor type that typically presents with low T cell infiltration and moderate tumor mutational burden. The response rate of immune checkpoint inhibitors (ICIs) targeting PD-1 as monotherapy is approximately 12% to 18%.
Mutations in the tumor genome cause tumors to express abnormal proteins that are not normally present in normal cell pools, also known as tumor neoantigens. Advances in next-generation sequencing technology have led to the development of personalized immunotherapies for individual cancer patients. Patients with innate immunity to tumor neoantigens often respond strongly to immune checkpoint inhibitors, which provides an initial rationale for combining immune checkpoint inhibitors with therapies that induce neoantigen-specific immunity.
On April 7, 2024, researchers from Geneos Therapeutics and Johns Hopkins University published a research paper entitled “Personalized neoantigen vaccine and pembrolizumab in advanced hepatocellular carcinoma: a phase 1 and 2 trial” in the journal Nature Medicine.
Results from the Phase 1/2 clinical trial of the personalized therapeutic cancer vaccine GNOS-PV02 (coded by plasmids for up to 40 tumor neoantigens) in combination with pembrolizumab (an anti-PD-1 monoclonal antibody) in advanced hepatocellular carcinoma showed an objective response rate of 30.6% (11/36 patients) in 36 patients with advanced hepatocellular carcinoma who had previously received too much tyrosine kinase inhibitor (mTKI), including 3 patients with complete response and 8 patients with partial response.
The objective response rate of 30.6% was nearly twice that of pembrolizumab alone (16.9%), demonstrating that personalized cancer vaccines can enhance the clinical response to anti-PD-1 therapy in patients with advanced hepatocellular carcinoma.
In preclinical studies, therapeutic cancer vaccines targeting mutation-associated neoantigens induced tumor-specific T cell responses and inhibited tumor growth.
Preliminary clinical trials of personalized therapeutic cancer vaccines (PTCVs) have also demonstrated the induction of neoantigen-specific immune responses in cancer patients.
Recently, data from a Phase 2b clinical trial of Moderna’s cancer vaccine mRNA-4157 in combination with pembrolizumab (an anti-PD-1 monoclonal antibody) in advanced melanoma showed that the combination significantly improved recurrence-free survival (RFS) compared to pembrolizumab alone, with a 49% lower risk of recurrence or death and a 62% lower risk of distant metastasis or death.
However, for tumor types that respond poorly to immunotherapy, such as hepatocellular carcinoma, it has not been proven whether vaccine-induced T cells are able to enter pre-existing tumors and induce tumor clearance in combination with anti-PD-1 therapy.
In this study, the research team conducted a single-arm, open-label, multicenter Phase 1/2 clinical trial in 36 patients with advanced hepatocellular carcinoma who had previously received too much tyrosine kinase inhibitor (mTKI) to investigate the therapeutic efficacy of GNOS-PV02, a personalized therapeutic cancer vaccine, in combination with pembrolizumab (an anti-PD-1 monoclonal antibody). The primary endpoints of this clinical trial are safety and immunogenicity, and the secondary endpoints are treatment efficacy and feasibility.
This personalized therapeutic cancer vaccine, GNOS-PV02, consists of a DNA plasmid encoding up to 40 tumor neoantigens that were determined by DNA and RNA sequencing and germ cell DNA sequencing of each patient’s tumor sample. GNOS-PV02 is co-formulated with another plasmid encoding the cytokine interleukin-12 (pIL-12), which acts as a vaccine adjuvant, via intradermal injection and is facilitated by an in vivo electroporation device. Intradermal injection of pIL12 results only in local and transient IL-12 production at the injection site and promotes locally induced cellular responses to expressed antigens.
The most common treatment-related adverse event was injection site reactions, which were observed in 15 (41.6%) of 36 patients. No dose-limiting toxicities or treatment-related ≥ grade 3 adverse events were observed, and the objective response rate was 30.6% (11/36), of which 8.3% (3/36) patients achieved complete response.
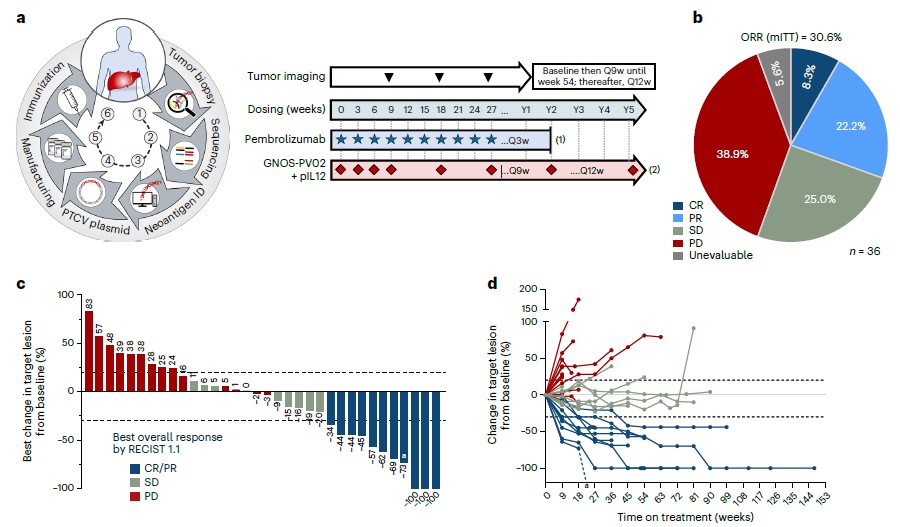
Fig. 1 The clinical response of GNOS-PV02.1
Clinical response correlates with the number of neoantigens encoded in the vaccine, and patients who receive a vaccine that encodes a larger number of neoantigens have better treatment outcomes. Further testing revealed that 19 of the 22 evaluable patients (86.4%) developed neoantigen-specific T cell responses. Multiparametric cell analysis showed that vaccine-specific CD4+ and CD8+ effector T cells were viable, proliferating, and killing. T cell receptor β chain (TCRβ) sequencing results showed clonal expansion and tumor infiltration of T cells enriched by the vaccine. Single-cell analysis shows clonal expansion of T cells with cytotoxic T cell phenotypes after treatment. Cyclability to vaccine-encoded neoantigens was confirmed by TCR-complementation-determining region cloning of expanded T cell clones in tumors after vaccination.
The results of these clinical trials support the mechanism of action of the personalized therapeutic cancer vaccine based on the induction of anti-tumor T cells, indicating that the personalized therapeutic cancer vaccine in combination with pembrolizumab (an anti-PD-1 monoclonal antibody) has clinical activity against advanced hepatocellular carcinoma.
Creative Biolabs offers a comprehensive suite of cancer vaccine services based on its advanced platforms for neoantigen prediction and in vitro evaluation.
- Personalized Neoepitope mRNA Cancer Vaccine Platform
- Modular NeoVax Platform for Cancer Vaccine
- Synthetic Long Peptides (SLPs) Based Neoantigen Cancer Vaccines
- Dendritic Cell (DCs) Based Neoantigen Cancer Vaccines
- Biomaterial-assisted Neoantigen Cancer Vaccines
- AI-aided Analysis Platform for Prediction of Tumor Neoantigen
- High-efficient NeoantigenIn Vitro Evaluation Platform
- Adoptive Neoantigen-activated T Cell Transfer Therapy
- NeoTCR-T Platform- T Cells with Tumor Neoantigen-specific T Cell Receptors
Reference
- Yarchoan, Mark, et al. “Personalized neoantigen vaccine and pembrolizumab in advanced hepatocellular carcinoma: a phase 1/2 trial.” Nature medicine (2024): 1-10.
