The complement system, a vital component of innate immunity and a potent promoter of inflammation, has a crucial role in host defense against pathogens and the development of central and peripheral nervous system disorders, including autoimmune, infectious, and degenerative diseases.
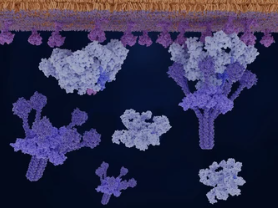
As a protein cascade, the complement system is activated by specific recognition molecules through a series of protein-protein interactions, culminating in the formation of a cytolytic pore. Complement precursor proteins are mainly synthesized by hepatocytes and then released into the bloodstream, where they are activated through three pathways: classical, alternative, and lectin, eventually forming the membrane attack complex (MAC).
The complement activation products play a pivotal role in linking the innate and adaptive immune systems by directly acting on receptors on T and B cells or by regulating dendritic cell function. Fine-tuned disruption is required for complement activation and control, which underlies the pathogenesis of several autoimmune neurological disorders and neurodegenerative diseases. Therefore, researchers are increasingly focusing on therapeutic approaches that target the complement system to prevent persistent tissue destruction in some refractory neurological diseases.
The Main Functions and Key Proteins of the Complement System
The complement system can be functionally divided into two main parts: the enzymatic cascade and the cleavage pathway. An enzymatic cascade produces the molecules required to initiate the cleavage pathway, during which the soluble protein undergoes a conformational change that enables it to insert into the lipid bilayer, eventually forming the MAC. The enzyme cascade’s primary function is the assembly of invertase, which drives the subsequent activation, amplification, and opsonization of complement. The cascade comprises three axes of activation: the classical pathway, the lectin pathway, and the alternative pathway, where proteolytic enzyme complexes activate each other in strict order.
The classical pathway begins with antibody-mediated activation of C1, leading to the formation of the C3 convertase C4bC2a complex. C3 convertase cleaves C3 to generate C3b, and C3b forms a complex with C4b and C2a, which is C5 convertase, which can cleave C5 to generate C5a and C5b. The lectin pathway, on the other hand, begins with the activation of MASP1 and MASP2 by oligomeric structures of mannose-binding lectin, ficolin, and collectin. Both pathways generate C5 convertase, which can cleave C5 to generate C5a and C5b. The alternative pathway, meanwhile, involves the interaction of C3 with factors B and D, leading to the cleavage of more C3 and perpetuating the process through the amplification loop.
All three pathways generate C5b, which initiates the formation of the MAC. C5b, along with surface-bound invertase, receives C6 and C7, and the complex must be translocated to the outer part of the lipid bilayer to successfully proceed with MAC formation. This results in a transmembrane complex that exposes lipophilic structures capable of binding C8 and C9, and the further association of the complex with 17 additional C9 molecules widens the inner pore size, resulting in a permeable MAC. CD59, a glycosylphosphatidylinositol-anchored protein, primarily mediates the control of MAC assembly to ensure protection from autocomplement attack and MAC formation.
Complement System and Nervous System Diseases
Dysfunction of the complement system, such as missing or excessive consumption of components, inappropriate control, or misdirection of autoantibodies, can lead to acute or chronic autoimmune and inflammatory neurological diseases. Complement-associated neurological disorders can result from complement protein dysfunction or abnormal activation of complement.
- Complement protein dysfunction
Dysfunction of complement activation predisposes to infections and autoimmune-like phenomena. The most severe neurological manifestations are caused by genetic defects in CD59 or mutations in its major ankyrin glycosylphosphatidylinositol, leading to the destruction of neural tissue by an uncontrolled autocomplement attack.

CD59 deficiency mainly contributes to the pathology of paroxysmal nocturnal hemoglobinuria (PNH), which, in turn, leads to neurological disease-like manifestations. Primary neurological diseases caused by CD59 deficiency are relatively rare, and only 13 patients have been reported so far, with symptoms manifesting as an acute significant motor demyelinating neuropathy accompanied by recurrent and aggravated conduction block of acute reflex paralysis, leading to secondary axonal injury, indistinguishable from recurrent Guillain-Barré syndrome (GBS) or chronic inflammatory demyelinating polyneuropathy (CIDP). C5 antibody treatment with Eculizumab can alleviate the patient’s symptoms.
Certain pathological conditions impair CD59 potency. For example, persistent hyperglycemia in diabetics can lead to increased glycosylation and impaired protein function, including CD59. Hyperglycemia itself also activates complement, and these effects may contribute to diabetes-related vascular and neurological complications.
- Abnormal complement activation
Circulating autoantibodies, especially antibodies of the IgG1 subclass, can mobilize complement when bound to antigens, leading to tissue damage. Antibodies of the IgG4 subclass cannot activate complement due to their low binding efficiency to C1q. However, over time, pathogenic IgG4 antibodies can induce autoimmune pathology by competing with natural antibodies for C1q binding sites, thereby delaying the autoimmune clearance of changes and aging.
Under physiological conditions, the blood-brain barrier normally restricts the entry of plasma proteins into the brain. As aging, mitochondrial dysfunction, and oxidative stress occur, leading to a leaky blood-brain barrier, IgG and complement components can enter the brain, leading to neurologic clinical manifestations. These indications also lead to the release of intracellular antigens that may be recognized by C1q, thereby activating complement. Complement can also be activated if C1q binds to the Fc portion of IgG and IgM antibodies bearing neuronal antigens such as gangliosides, glial fibrillary acidic protein, or various neuronal channels or receptors.
Complement activation also occurs in brains with an intact blood-brain barrier. Studies in animal models have shown that microglia and astrocytes synthesize and secrete most complement proteins. Under physiological conditions, the protective role of complement in the brain includes scavenging excess neurotransmitters, clearing aging proteins, pruning synapses, and regulating adult neurogenesis.
- Nerve Root and Peripheral Nervous System DiseasesGBS.
GBS is an autoimmune peripheral neuropathy characterized by demyelinating lesions of peripheral nerves and nerve roots and infiltration of inflammatory cells in small vessels. In various GBS variants, particularly acute motor axonal neuropathy, acute motor and sensory axonal neuropathy, and Miller-Fisher syndrome, ganglioside antibodies target myelinated fibers or axons, causing complement activation, MAC formation, disruption of sodium channel expression, and conduction block. Deposition of C3b on the surface of Schwann cells leads to myelin damage, followed by the infiltration of activated macrophages and T cells. Ganglioside antibodies produce a GBS-like phenotype by damaging perisynaptic Schwann cells in a mouse model of ganglioside-mediated passive transfer of neuropathy, but this effect occurs only in the presence of human complement. In these models, eculizumab effectively prevented dysfunction and neurological damage. In in vitro studies, quantitative assessment of C3 uptake revealed that C3 fragments were deposited on sensitized targets to a greater extent in GBS patient sera than in healthy control sera, an observation that supports the notion that C3b and MAC deposition play a role in neural injury.
CIDP. In CIDP, complement and IgG are deposited on myelinated fibers, and serum levels of terminal complement-activating components increase with disease severity. However, dense myelin complement fixation antibodies that account for active demyelination and conduction block have not been identified in CIDP. Studies of the Ranvier lymph nodes have shown that up to 10% of patients with CIDP have antibodies to Neurofascin 155, Contactin 1, and Contactin-associated protein 1 (CASPR1), which are required to maintain lymph node architecture, but instead of causing the complement fixation and macrophage-mediated demyelination seen in classical CIDP, these IgG4 antibodies prevent protein-protein interactions, resulting in non-inflammatory structural nodal protein adhesions. Most patients with these antibodies did not respond to intravenous C3-inhibiting immunoglobulin (IVIg) but responded to treatment with rituximab, an anti-CD20 monoclonal antibody targeting B cells.
Multifocal Motor Neuropathy (MMN). MMN is a distinct motor neuropathy associated with conduction block characterized by distal asymmetry and predominantly upper extremity weakness without substantial paresthesias in up to 50% of patients and the presence of IgM antibodies to the ganglioside GM1. These antibodies activate the classical pathway of complement, and complement activity correlates with disease severity. In induced pluripotent stem cell-derived MMN models, the interaction of these antibodies with complement interferes with motor neuron function, leading to cell damage and death.
Paraproteinemic Neuropathy. In IgM paraproteinemic neuropathy associated with myelin-associated glycoprotein (MAG) and sulfoglucuronyl paragloboside antibodies, sural nerve biopsy showed anti-MAG IgM and complement deposition on myelinated fibers, suggesting that complement activation is required to induce demyelination. In addition, skin biopsies from patients showed deposition of anti-MAG and C3d IgM in myelinated fibers, supporting the notion that complement plays a role in splitting the myelin layer and inducing nerve fiber loss. However, to date, no complement-related therapy has been tested in paraproteinemic neuropathies.
Neuropathic Pain. Inflammation triggered by the complement cascade may drive neuropathic pain, but this hypothesis is controversial. Anaphylatoxins C3a and C5a, especially C5a, may be the link between complement activation and pain. The binding of C5a to its receptor, C5aR1, triggers the release of cytokines that attract macrophages and neutrophils. Drugs that prevent C5a from binding to C5aR1, such as PMX53, reduce pain in animal models, but these results have not yet translated to the clinic.
