Alzheimer's Disease
Alzheimer's disease (AD) is a progressive neurodegenerative disease mainly manifested as memory impairment and cognitive decline, and it is the most common form of dementia. It is estimated that around 50 million people worldwide are living with AD or other forms of dementia, and this number is growing. AD not only imposes significant physical and mental burdens on patients and families but also creates substantial economic pressure on society and the medical system. The exact pathogenesis of AD is unknown, but it is known to be associated with abnormal deposits of proteins such as amyloid plaques and neurofibrillary tangles. Amyloid plaques are extracellular deposits formed by the aggregation of amyloid beta (Aβ), while neurofibrillary tangles are intracellular deposits formed by the aggregation of hyperphosphorylated tau protein. Abnormal deposition of these proteins can lead to neuronal dysfunction and death, causing atrophy of structures such as the cerebral cortex and hippocampus. The occurrence of AD is related to genetic factors to a certain extent, and gene variations associated with AD have been found on chromosomes 1, 14, 19, and 21. For example, variations such as the Down syndrome critical region gene (DSCR) on chromosome 21 may be associated with AD, as individuals with Down syndrome often develop clinical manifestations of early-onset AD.
Clinical Manifestations
The clinical manifestations of AD mainly include memory impairment, language impairment, visuospatial dysfunction, executive dysfunction, emotional, and behavioral changes, among others. These manifestations are associated with atrophy of structures such as the cerebral cortex and hippocampus, primarily involved in memory and cognitive processes. Memory impairment is the earliest and most prominent symptom of AD, usually manifested as a decline in recent memory, meaning the forgetting of recent events or learned information. As the disease progresses, long-term memory, the forgetting of past experiences or knowledge, can also be affected. Memory impairment can cause patients to face difficulties in daily life, such as not finding things, asking the same questions repeatedly, or getting lost.
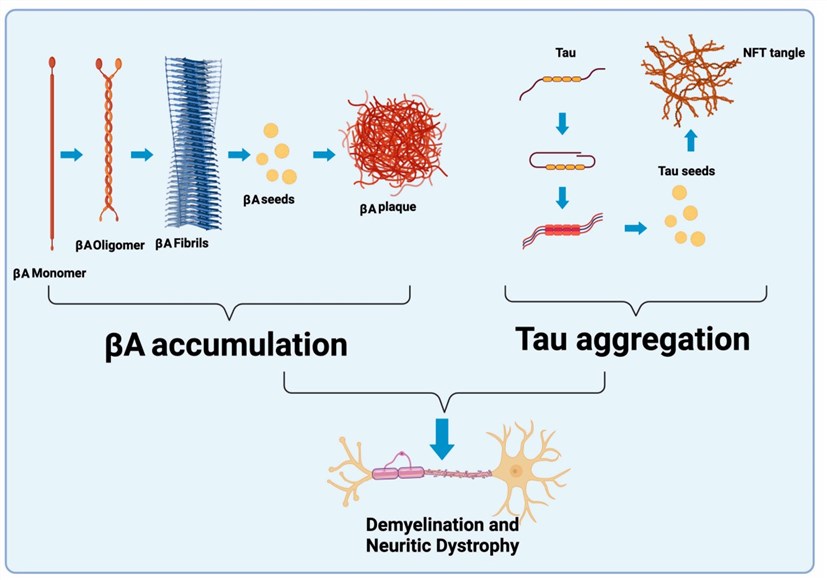 Fig.1 Schematic representation of AD pathology. (Tamburini B, 2023)
Fig.1 Schematic representation of AD pathology. (Tamburini B, 2023)
The clinical manifestations of AD are usually divided into three stages: early, middle, and late stages, each with different characteristics and severity. The early stage is mainly characterized by mild memory impairment and a slight decline in daily life ability. The middle stage is marked by moderate memory impairment and a noticeable decline in daily life ability, along with other cognitive impairments such as language impairment, visuospatial dysfunction, emotional and behavioral changes, as well as non-cognitive symptoms. The late stage manifests as severe memory impairment and a complete loss of daily life ability, accompanied by severe cognitive and non-cognitive symptoms such as executive dysfunction and physical function decline.
Diagnosis and Treatment Methods
The clinical diagnosis of AD is primarily based on the patient's symptoms, physical examination, neuropsychological tests, imaging examinations, and laboratory tests. Currently, there is no single examination method that can confirm the diagnosis of AD, but a comprehensive diagnosis is required based on the results of multiple tests. Symptoms serve as the foundation for diagnosing AD, often involving an understanding of changes in the patient's memory, cognition, emotion, and behavior as described by the patient or family members. To objectively assess the patient's symptoms, various scales or questionnaires can be utilized, such as the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), and Alzheimer's Disease Assessment Scale Table (ADAS). Physical examination is a crucial step in the diagnosis, primarily to rule out other physical conditions that may cause similar symptoms. Neuropsychological testing is vital to evaluate the patient's various cognitive functions, including attention, memory, language ability, and executive ability. Imaging examinations serve as auxiliary methods, observing changes in brain structure and function, and ruling out other brain diseases with similar symptoms. Laboratory tests are supplementary, focusing on detecting AD-related biomarkers in the patient's blood or cerebrospinal fluid.
Currently, there is no cure for AD, and the main focus of treatment is to relieve symptoms and improve the quality of life. Treatment methods for AD include drug therapy, non-drug therapy, and gene therapy. Drug therapy, the most commonly used treatment, involves cholinesterase inhibitors and NMDA receptor antagonists to increase neurotransmitter levels or reduce neuronal damage. Non-drug treatments are important and may include cognitive training, behavioral intervention, and lifestyle changes to improve cognitive function or reduce emotional and behavioral problems. Gene therapy, an emerging treatment, utilizes technologies such as gene editing or gene transfer to repair or replace abnormal genes or express beneficial genes. Gene editing involves the use of specific nucleases or nucleic acid guidance systems (such as CRISPR-Cas9) to cut or repair target gene sequences, eliminating or correcting mutations associated with AD. Gene transfer refers to the introduction or expression of target gene sequences through specific vectors (such as adeno-associated viruses), aiming to increase or restore functions related to AD. Gene therapy holds promise for the fundamental treatment of AD.
References
- Montine TJ, et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta Neuropathol. 2012 Jan;123(1):1-11.
- McKhann GM, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011 May;7(3):263-9.
- Tamburini B, et al. Emerging Roles of Cells and Molecules of Innate Immunity in Alzheimer's Disease. Int J Mol Sci. 2023 Jul 25;24(15):11922.
- Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002 Jul 19;297(5580):353-6.
- Khan S, et al. Recent Advancements in Pathogenesis, Diagnostics and Treatment of Alzheimer's Disease. Curr Neuropharmacol. 2020;18(11):1106-1125.
- Lott IT, et al. Beta-amyloid, oxidative stress and down syndrome. Curr Alzheimer Res. 2006 Dec;3(5):521-8.
- Dubois B, et al. Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol. 2014 Jun;13(6):614-29.
- Jack CR Jr, et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018 Apr;14(4):535-562.
- Cummings JL, et al. Effect size analyses of souvenaid in patients with Alzheimer’s disease. J Alzheimers Dis. 2017;55(3):1131-1139.
- Birks J, Harvey RJ. Donepezil for dementia due to Alzheimer’s disease. Cochrane Database Syst Rev. 2018 Jun;6(6):CD001190.
- McShane R, et al. Memantine for dementia. Cochrane Database Syst Rev. 2006 Apr;(2)(2):CD003154.
- Liu Q, et al. Gene therapy for Alzheimer’s disease: where are we now? Mol Neurodegener. 2020 Feb;15(1):15.
