TCR-T cell therapy is a type of immunotherapy for cancer that has shown promise in treating myeloma, myeloid malignancies, and solid tumors. The underlying theory of immunotherapy is that immune cells, such as T cells, can recognize and eliminate cancer cells. TCR-T therapy seeks to accomplish this by genetically modifying T cells to recognize and attack cancer cells, making it a powerful tool in the fight against cancer.
T-cell receptor (TCR) is a protein complex composed of an α and β chain located on the surface of T cells, which recognizes and binds to fragments of antigens presented by major histocompatibility complex (MHC) molecules. Although each TCR is specific to one antigen, the affinity between normal TCRs and antigens is relatively low, indicating weak ability to recognize and kill cancer cells. In TCR-T cell therapy, the modified T cells used have much higher affinity. Genetically modified T cells can express chimeric TCRs, consisting of three parts: an ectodomain with a single-chain fragment variant (scFv) for antigen recognition, a transmembrane domain, and an endodomain that includes a CD3ζ chain with three immunoreceptor tyrosine-based activation motifs (ITAMs). The modified T cells can recognize human antigen-peptide complexes on cancer cells and transmit antigen-stimulating signals through phosphorylation of ITAM, which initiates effector functions such as proliferation, cytokine secretion, and cytolysis via the secretion of perforin and granzyme. TCR-T cells can activate the immune effects of T cells and specifically recognize tumor-associated antigens to eliminate tumor cells more effectively.
According to Liu et al.'s research in 2022, TCR-T technology has undergone four iterations of development. Initially, isolated tumor antigen-specific T cell subgroups were amplified in vitro and re-infused into the same patient to attack tumors. However, producing this therapy on an industrial level proved difficult due to inter-individual variations of T cells. In the second iteration, TCR gene sequences were transduced into peripheral T cells from patients, allowing for TCR-T cell production.
The third iteration focused on improving the therapeutic effects of TCR-T cells by optimizing the affinity of their TCRs for tumor cells. In the fourth and current iteration, TCR-T cell treatment focuses on the safety of patients and boosting their anticancer immune system. This includes targeting new antigens, manufacturing new engineered or modified TCRs, and creating a safety switch for endo-suicide genes.
TCR-T therapy has many advantages. For example, it is free from the limits of surface antigen expression in the target cells. Strategic selection of substrate cells can enhance the transportation, amplification, durability, and memory functions of TCR-T cells, and it can form a TCR-T cell system with a synthetic costimulatory circuit. However, this therapy method has not been approved by regulatory authorities, even though it is considered a potential cancer immunotherapy. There are many examples of successful and unsuccessful clinical trials. The earliest clinical trials for TCR-T-cell therapy were in 1999. According to the clinical trials published on ClinicalTrials.gov updated by June 11, 2018 and searched by Zhang & Wang, the most frequently studied cancer type is melanoma, which is probably because of the relatively high frequency of melanoma cases. Leukemia, gastrointestinal cancers, and hematological malignancies are followed.
There are various unique strategies to engineer T cells, each of these strategies has unique features that cater to different kinds of cancers. Antibody-coupled TCR-T cells are generated by engineering T cells to couple with an antibody that can specifically bind to tumor antigens. This mode of therapy allows for the targeted killing of cancer cells while sparing healthy cells in the body. TCR fusion construct (TRuC) T cells are T cells engineered with a fusion protein that combines both the TCR and an antibody-binding domain on a single molecule. This allows the T cells to better recognize and attack cancer cells more efficiently. In addition, researchers have developed single-chain TCR (scTCR)-redirected T cells to address the issues related to the pairing of endogenous TCRs.
There are many clinical studies that highlight the potential of TCR-T therapy and further research in this field. For example, a clinical trial (NCT00910650) investigated the adoptive transfer of MART-1 TCR transgenic lymphocytes together with MART-1 peptide-pulsed dendritic cell vaccination in HLA-A2.1 patients with metastatic melanoma. Autologous TCR transgenic cells were manufactured in 6 to 7 days using retroviral vector gene transfer and were reinfused with or without prior cryopreservation. The results showed that 9 of the 13 treated patients (69%) exhibited tumor regression. However, two patients experienced serious adverse respiratory distress events and required intervention.
Another clinical trial administered autologous TCR-transduced T cells plus 720,000 iU/kg of interleukin-2 to patients with NY-ESO-1-positive tumors after preparative chemotherapy. The study found that in four out of six patients with synovial cell sarcoma and five out of eleven patients with melanoma bearing tumors expressing NY-ESO-1, tumor regression occurred. Two of eleven patients with melanoma demonstrated complete regressions that persisted after 1 year, and a partial response lasting 18 months was observed in one patient with synovial cell sarcoma. While the treatment led to tumor regression and disease remission to some extent, it may also result in other clinical symptoms.
There have also been failed clinical trials in TCR-T cell therapy. One such trial involved administering autologous T lymphocytes genetically engineered to express a murine TCR against human carcinoembryonic antigen (CEA) to three patients with metastatic colorectal cancer that was refractory to standard treatments. While all patients experienced decreases in serum CEA levels (ranging from 74 to 99%), and one patient showed objective regression of cancer metastases in the lung and liver, all three patients suffered from severe transient inflammatory colitis that represented a dose-limiting toxicity. In another study by Morgan et al. in 2013, nine cancer patients were treated with adoptive cell therapy using autologous anti-MAGE-A3 TCR engineered T cells, and five patients experienced clinical regression of their cancers. However, three patients experienced mental status changes beginning 1-2 days post-infusion, and two patients lapsed into comas and subsequently died. These failed trials demonstrate the need to avoid severe clinical responses even if there appears to be a response of tumor regression.
Although TCR-T cell therapy has the potential to be an effective cellular immunotherapy for cancer treatment, it still faces many challenges. One of the obstacles is TCR mismatch, which can occur due to differences between the exogenous TCR αβ gene sequence introduced by genetically modified T cells and the endogenous TCR αβ gene sequence, causing the attack of healthy cells. Additionally, the risk of false targeting caused by increased TCR affinity should be minimized or avoided. Nonspecific cytotoxicity is another obstacle, as TCR-T cells may attack healthy tissues expressing an antigen or epitope similar to the intended target, leading to severe reactions. Adverse reactions such as cytokine storms should also be eliminated. Finally, manufacturing cost and complexity, T cell persistence, immunosuppressive tumor microenvironment, and tumor intrinsic escape mechanisms should also be addressed.
References
For any technical issues or product/service related questions, please leave your information below. Our team will contact you soon.
All products and services are For Research Use Only and CANNOT be used in the treatment or diagnosis of disease.
 NEWSLETTER
NEWSLETTER
The latest newsletter to introduce the latest breaking information, our site updates, field and other scientific news, important events, and insights from industry leaders
LEARN MORE NEWSLETTER NEW SOLUTION
NEW SOLUTION
CellRapeutics™ In Vivo Cell Engineering: One-stop in vivo T/B/NK cell and macrophage engineering services covering vectors construction to function verification.
LEARN MORE SOLUTION NOVEL TECHNOLOGY
NOVEL TECHNOLOGY
Silence™ CAR-T Cell: A novel platform to enhance CAR-T cell immunotherapy by combining RNAi technology to suppress genes that may impede CAR functionality.
LEARN MORE NOVEL TECHNOLOGY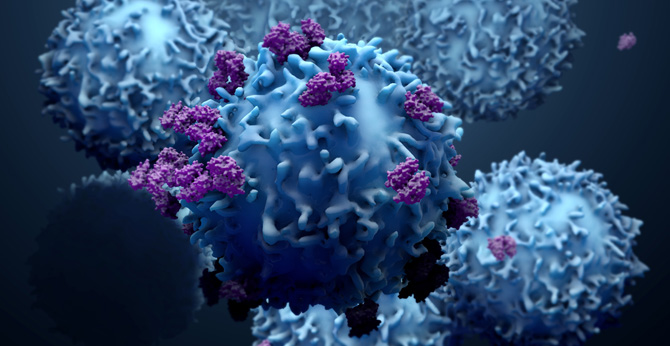 NEW SOLUTION
NEW SOLUTION
Canine CAR-T Therapy Development: From early target discovery, CAR design and construction, cell culture, and transfection, to in vitro and in vivo function validation.
LEARN MORE SOLUTION