Natural killer (NK) cells have been considered to have the ability to kill viral infections and malignant cells without activation. Unlike B and T cells, NK cells do not need somatic gene rearrangement to produce highly specific receptors that recognize target cells. Instead, mature NK cells retain a large number of cytotoxic particles containing perforin and granzyme, as well as IFN γ mRNA, which can be translated after stimulation. Once the balance between inhibitory signal and activation signal in NK cells is broken and NK cells tend to activate, NK cells can form synapses with target cells, releasing perforin and granzyme to cleave target cells and produce IFN γ. In addition, NK cells can initiate death signal transduction in target cells through death receptor/ligand connections. The cytotoxicity and inflammatory cytokines they produce enable NK cells to play an important role in different environments of cancer immunotherapy.
NK Cells and Tumor Immune Surveillance & Control
NK cells are considered to be a group of powerful immune effectors in tumor surveillance and control. However, evidence of abnormal NK cell function has been observed in many cancer patients, and many tumors have established pathways to escape immune surveillance through NK cells. Therefore, it is possible to achieve promising clinical results by manipulating NK cells to reverse their failures caused by a variety of inhibitory mechanisms.
NK cells can lyse tumor cells without prior exposure. When attacked by a tumor, NK cells are activated in two main ways. The reduced expression of MHC class I in tumor cells activates NK cells through the lack of inhibitory signals, which is known as the "missing-self" theory. Tumor cell stress induces the expression of receptor ligands in activated NK cells, which leads to the activation of NK cells.
Functional defects in NK cells lead to an increase in tumor incidence and virus infection. Individuals who showed lower NK cell activity were considered to have a higher risk of tumorigenesis. Tumor cells escape from NK cell immune surveillance through two main mechanisms: 1. The activation signal decreased; 2. The inhibitory signal transmitted to NK cells increased. In some studies, it has been observed that soluble NKG2D ligands fall off from tumor cells, which may prevent NK cells from recognizing tumor cells with the ligand. The decreased expression of DNAM-1 in NK cells in acute myeloid leukemia means that the expression of activated receptors in NK cells can be down-regulated to inhibit the activation of NK cells. In addition, tumor cells can down-regulate the expression of receptor ligands in activated NK cells in tumor microenvironment, which is also a protective strategy for tumor cells to retain HLA expression. When a tumor escapes immune surveillance, the tumor evasion occurs. Negative regulation of immune cells and inhibitory molecules may contribute to the further inhibition of NK cells. The above mechanisms used by the tumor inhibit the activation of NK cells, and even the phenotypic changes of NK cells can be observed in the tumor site. Therefore, the restoration of anti-tumor activity of NK cells is very important for the establishment of host anti-cancer immunity, which is the main goal of cancer immunotherapy.
 Figure 1. Mechanism of tumor immune escape from NK cells. (Chin J Cancer Res, 2018)
Figure 1. Mechanism of tumor immune escape from NK cells. (Chin J Cancer Res, 2018)
Therapeutic Strategies for Restoring Anti-tumor Activity of NK Cells
—Therapeutic Antibodies Targeting NK Cells
In cancer patients, the anti-tumor function of NK cells is usually impaired, and the strategy of restoring NK cell function can be understood as two pathways: increasing activation factors or decreasing inhibitory factors. This is determined by the basic characteristics of NK cell activation. NK cell adoptive cellular immunotherapy can provide a large number of activated NK cells to directly supplement or replace NK cells with abnormal function in cancer patients. Cytokines are used to enhance the survival of NK cells in vitro or in vivo. Retargeting strategies, including the use of therapeutic antibodies, bispecific proteins and NK cells that express chimeric antigen receptor (CAR-NK), have been used to enhance the specificity of NK cells to eliminate cancer. In addition, genetic modification of NK cells and oncolytic virus therapy have been introduced to promote the anti-tumor activation of NK cells.
 Figure 2. Immunotherapeutic strategies for restoring NK cell anti-tumor responsiveness. (Chin J Cancer Res, 2018)
Figure 2. Immunotherapeutic strategies for restoring NK cell anti-tumor responsiveness. (Chin J Cancer Res, 2018)
Specific monoclonal antibodies (mAbs) that recognize tumor cell surface antigens are used in cancer treatment. These therapeutic mAbs target and attack tumor cells through a variety of mechanisms, including guiding toxic molecules to target cells, inhibiting the proliferation of target cells, blocking inhibitory signals against immune cells, and guiding immune cells to kill targets through antibody-dependent cellular cytotoxicity (ADCC). Some novel antibodies, such as bispecific antibody (bsAbs), play a role by promoting the formation of conjugates between target cells and NK or T cells.
 Figure 3. NK cells and tumor-targeted therapeutic antibody-mediated ADCC. (Nature Reviews Cancer, 2016)
Figure 3. NK cells and tumor-targeted therapeutic antibody-mediated ADCC. (Nature Reviews Cancer, 2016)
In the context of tumor-targeted monoclonal antibody therapy, the anti-tumor efficacy of many mAbs has been shown to be NK cell dependent. Human NK cells can express FcγRIIC/CD32c and FCγRIIIA/CD16a, which bind to the Fc portion of human immunoglobulins. FcγRIIIA is usually associated with FcϵRI-γ chains or CD3-ζ chains in the cell membrane, or with a heterodimer of these two chains. Unlike most activated receptors on NK cells, FcγRIIC has an immune tyrosine-based activating motif (ITAM) in its own cytoplasmic tail. Upon FcγR binding, these ITAMs are phosphorylated, and through the signal transduction mechanism, NK cell degranulation, cytokine secretion, and finally tumor cell lysis occur. Antibody-dependent NK-mediated tumor killing occurs through several different pathways, including the exocytosis of cytotoxic granules, the death receptor signaling of TNF family, and the release of proinflammatory cytokines, such as IFNγ. The absorption of perforin and granzymes by target cells and the transduction of TNF death receptor signaling lead to apoptosis of target cells, while IFNγ released by NK cells activates nearby immune cells to promote antigen presentation and adaptive immune response.
The tumor-specific mAbs listed in the table below have been shown to work at least in part in preclinical or clinical models through ADCC.
Table 1. Representative tumor-antigen targeting monoclonal antibodies functioning through ADCC
| Antibody | Targeting antigen | Strategy | Condition | Stage of clinical development |
| Rituximab | CD20 | ADCC | B cell NHL; CLL | FDA approved |
| Ofatumumab | CD20 | ADCC | CLL | FDA approved |
| Trastuzumab | HER2 | ADCC | HER2+ breast cancer; HER2+ gastric-esophageal junction carcinoma | FDA approved |
| Cetuximab | EGFR | ADCC | Advanced SCCHN | FDA approved |
| Dinutuximab | GD2 | ADCC | Pediatric neuroblastoma | FDA approved |
| Elotuzumab | SLAMF7 | ADCC | MM | FDA approved |
| Obinutuzumab | CD20 | Optimized ADCC | CLL | FDA approved |
Dinutuximab is a chimeric mAb, that contains the human constant part of IgG1 and fusion protein of disialoganglioside (GD2) reactive variable part of mouse 14.18 mAb. It was approved by the US Food and Drug Administration (FDA) in 2015 and is used as a first-line treatment for children with high-risk neuroblastoma. Dinutuximab is produced in murine myeloma cell line. Its mechanism is based on the binding of cell surface glycolipid GD2 and lysis of GD2-expressed cells via ADCC and complement-dependent cytotoxicity (CDC).
Trastuzumab is a humanized anti-HER2 mAb, that can be used to treat HER2-positive breast cancer and many other types of cancer in which HER2, the member of the human epidermal growth factor receptor (EGFR) family are overexpressed. Trastuzumab was first approved by FDA in 1998 for the treatment of HER2 positive metastatic breast cancer. In addition to preventing the dimerization of HER2, trastuzumab has also been shown to mediate ADCC against HER2 positive tumor cells in vitro, and the main effector cells are NK cells expressing FcγRIIIA. In the xenotransplanted breast tumor model, the mutant trastuzumab, which lost the ability to bind to FcγR, lost its anti-tumor activity, which indicated that ADCC was involved in the anti-tumor effect of anti-HER2 mAb therapy in vivo. In addition, some experimental data show that Fc receptor recognition is part of the anti-tumor efficacy of trastuzumab.
Cetuximab is a chimeric mAb, approved by FDA for the treatment of cancers that express EGFR, including metastatic colorectal cancer (mCRC), metastatic non-small cell lung cancer and head and neck cancer. It responds to human EGFR and interferes with tumor growth by inhibiting growth factor-activated receptors. In vitro studies have shown that some of the anti-tumor activities of cetuximab are mediated by ADCC, and the in vitro ADCC mediated by cetuximab is associated with the FcγR polymorphism of NK cells in effect donors. In addition, both in vitro and some clinical data suggest that cetuximab-mediated ADCC through NK cells may contribute to its anti-tumor activity.
Rituximab is a chimeric IgG1 mAb targeting CD20. There are many mechanisms that can explain the anti-tumor effect of rituximab: complement-dependent cytotoxicity (CDC), direct target cell apoptosis, antibody-dependent phagocytosis and ADCC. Clinical evidence shows that the effect of FCγRIIIA on NK cells plays an important role in the anti-tumor effect of rituximab. Modifications have been made to improve the binding affinity of therapeutic anti-CD20 mAb to activating Fc receptors, in hopes of maximizing the ADCC function of this mAb therapy. Obinutuzumab, the first humanized anti-CD20 mAb engineered by Fc glycosyl, induced stronger ADCC in vitro and guided the death of target cells. Compared with rituximab, obinutuzumab also induced better anti-tumor activity in the mouse model of lymphoma xenotransplantation.
Blocking immune checkpoints is a promising strategy for cancer treatment. Because the anti-tumor activity of NK cells can also be reduced by inhibiting the signal transduction of receptors, inhibitory NK cell receptor antagonists were developed to enhance the anti-tumor activity of NK cells. These studies focus on the main inhibitory receptors of NK cells, including KIR, NKG2A and ILT.
KIRs inhibit NK cell activation by engaging HLA. Therefore, KIR antagonism is a promising strategy to block the checkpoint of NK cells. It has been shown that the variability of KIR gene indicates a response to monoclonal antibodies against EGFR. Lirilumab is a complete human monoclonal anti-KIR antibody that can block three major KIR (KIR2DL-1, -2 and-3). In vivo and in vitro, it can enhance the cytotoxicity of HLA-matched acute myeloid lymphoma mother cells mediated by NK cells.
Another important inhibitory receptor in NK cells is NKG2A, which forms a disulfide-linked heterodimer with CD94. NKG2A competes with NKG2C, the activated receptor of NK cells, to recognize HLA-E. NKG2A can inhibit the anti-tumor function of NK cells in many tumor types. Monalizumab is a blocking antibody to NKG2A, and clinical trials of the monoclonal antibody are under way. As a monotherapy, its efficacy is also being further evaluated.
Indoleamine 2,3-dioxygenase (IDO) and adenosine (ADO) are inhibitors of NK cell activity. IDO can inhibit the expression of NKG2D and NKp46 on NK cells and reduce the cytotoxicity of NK cells. It was also found that ADO damaged the anti-tumor activity of NK cells. CD39 and CD73 are membrane-bound extracellular enzymes that catalyze the transformation of ATP to AMP, upstream of IDO and ADO. They are expressed in regulatory immune cells and several types of tumor cells. The expression of CD73 on tumor infiltrating NK cells is related to the inhibition of NK cell activity. Antibodies have been produced to block CD39 and CD73, and both anti-CD39 and anti-CD73 have increased the cytotoxicity of NK cells to ovarian cancer cells in vitro. These CD39 and CD73 blocking antibodies represent another set of candidates for immune checkpoint blockade therapy that is expected to restore the viability of NK cells.
Recently, many bispecific antibodies (bsAbs) targeting NK cells have been produced. Like all other bsAb, these bsAb associated with NK cells show two binding specificity. One binding fragment is specifically connected to the NK cell activated receptor, and the other binding fragment is specifically connected to the tumor-associated antigen (TAA). They are also known as bispecific killer cell engagers (BiKEs), that can promote NK cell-mediated cytotoxicity. In theory, all NK cell activated receptors can be used as targets. However, so far, only FcγRIIIA has been selected as the target for these bsAbs, which may be due to the successful construction of anti- FcγRIIIA antibody 3G8, a functional antibody agonist. CD16A is an activated receptor with low affinity to Fc fragment of immunoglobulin. It is responsible for ADCC mediated by NK cells. The receptor associates innate immunity with adaptive immunity through the participation of IgG and combines the specificity of NK cells. In addition, NK cell-related bsAbs have been extended to trispecific and tetraspecific antibodies to improve the activation, proliferation and survival of NK cells and induce anti-tumor cytotoxicity of NK cells.
References
For any technical issues or product/service related questions, please leave your information below. Our team will contact you soon.
All products and services are For Research Use Only and CANNOT be used in the treatment or diagnosis of disease.
 NEWSLETTER
NEWSLETTER
The latest newsletter to introduce the latest breaking information, our site updates, field and other scientific news, important events, and insights from industry leaders
LEARN MORE NEWSLETTER NEW SOLUTION
NEW SOLUTION
CellRapeutics™ In Vivo Cell Engineering: One-stop in vivo T/B/NK cell and macrophage engineering services covering vectors construction to function verification.
LEARN MORE SOLUTION NOVEL TECHNOLOGY
NOVEL TECHNOLOGY
Silence™ CAR-T Cell: A novel platform to enhance CAR-T cell immunotherapy by combining RNAi technology to suppress genes that may impede CAR functionality.
LEARN MORE NOVEL TECHNOLOGY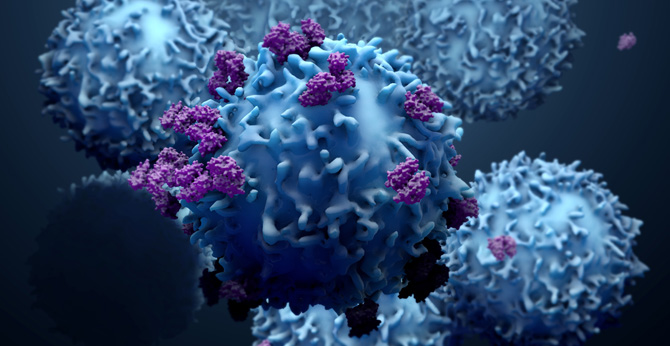 NEW SOLUTION
NEW SOLUTION
Canine CAR-T Therapy Development: From early target discovery, CAR design and construction, cell culture, and transfection, to in vitro and in vivo function validation.
LEARN MORE SOLUTION