Therapeutic Exosomes for Bronchopulmonary Dysplasia
Bronchopulmonary Dysplasia (BPD) is one of the important causes of neonatal death. Several studies have shown that mesenchymal stem cell-derived exosome (MSC-exo) can treat BPD and has entered the clinical stage. Creative Biolabs has been paying attention to the field of exosome drugs and has been committed to providing the latest exosome research technology to advance the research of exosome drugs for the treatment of BPD.
Bronchopulmonary Dysplasia (BPD)
BPD is a common chronic lung disease in premature infants. Deoxygenation is difficult in premature infants after prolonged reliance on mechanical ventilation. Therefore, this dyspnea causes further damage to the immature lung, activates the immune response, causes a disorder of inflammatory and anti-inflammatory factors in the lung, and causes damage or depletion of pulmonary stem cells. Further, these processes lead to pulmonary fibrosis, simplification of alveolar architecture, abnormal pulmonary angiogenesis, and persistent airway inflammation. Ultimately, the entire dynamic process leads to BPD. Due to the improvement of technologies such as non-invasive ventilation, lung-protective mechanical ventilation, and the application of pulmonary surfactant, the survival rate of premature infants under 28 weeks has gradually increased. But the incidence of BPD remains high. BPD has become a hot and difficult point of concern in neonatal intensive care units.
Therapeutic Exosomes for BPD
Studies have found that mesenchymal stem cells (MSCs) can regulate immunity, reduce lung fibrosis and inflammation, enhance the regeneration and repair of lung cells, reduce pulmonary hypertension, and bring hope for the cure of BPD. However, some studies have pointed out that there is no obvious engraftment of MSCs in the lung. This suggests that MSCs may function in a paracrine manner. MSC-exo is a physiologically relevant and powerful component of the MSC secretome, with similar biological functions to MSCs. MSC-exo instead of MSC therapy also avoids most of the safety concerns associated with cell therapy. Recently, studies have pointed out that the use of MSC-exo can treat BPD. Lung macrophages are key mediators of the lung immune response and play an important regulatory role in the inflammatory response of BPD.
A research group has treated BPD model mice with MSC-exo derived from human umbilical cord jelly and human bone marrow. They have found that MSC-exo is easily absorbed by alveolar macrophages. MSC-exo can improve BPD, lung function, and fibrosis, reduce pulmonary vascular remodeling and alleviate pulmonary hypertension by inhibiting the pro-inflammatory "M1" state of macrophages while enhancing the anti-inflammatory "M2-like" state. In addition, MSC-exo has anti-inflammatory and pro-angiogenic effects, preventing the disruption of alveolar growth and increasing the number of small blood vessels in a neonatal rat model of BPD induced by hyperoxia exposure for 14 days. Intratracheal administration of MSC-exo for BPD has entered clinical phase I. Alveolarization in mice generally begins on the postnatal fifth day. MSC-exo treatment has been given on the fourth day after birth in BPD model mice. When returned to room air for 1 week, most of the hyperoxia-induced dysregulation of lung gene expression has returned to normal. MSC-exos treatment on the 18th day after birth and continuous treatment from the 18th day to the 39th day after birth restored the lung structure and reduced pulmonary fibrosis in BPD model mice. These data suggest that MSC-exo is effective for both early prevention and late treatment of BPD.
TSG-6 in MSC-exo is an important therapeutic BPD molecule. Studies have shown that TSG-6 in MSC-exo attenuates lung inflammation and other BPD-related pathological features by antagonizing the inflammatory effects of tumor necrosis factor α (TNF-α) and interleukin-1 (IL-1) and participating in the negative feedback of the highest levels of TSG-6.
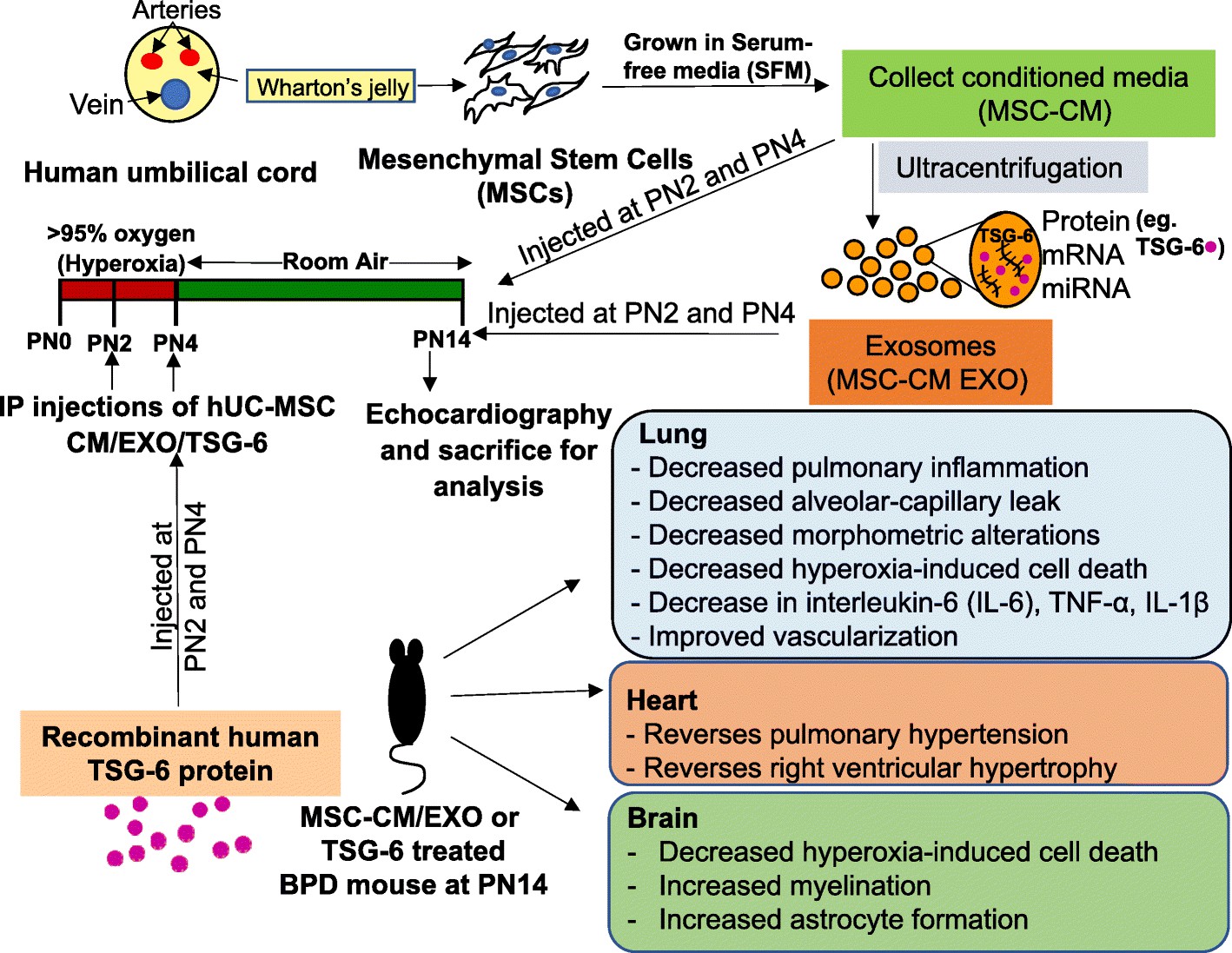 Fig.1 Schematic representation of MSC-CM/EXO/TSG-6 treatment regimen and outcomes in the mouse model of BPD.1,2
Fig.1 Schematic representation of MSC-CM/EXO/TSG-6 treatment regimen and outcomes in the mouse model of BPD.1,2
Creative Biolabs has been exploring disease-related exosome drug research with customers, providing customers with the most comprehensive and high-quality one-stop service for exosome research. You can always contact us to discuss your thoughts and ideas. Our most professional team of scientists will help you advance BPD-related exosome drug discovery.
References
-
Chaubey, S.; et al. Early gestational mesenchymal stem cell secretome attenuates experimental bronchopulmonary dysplasia in part via exosome-associated factor TSG-6. Stem Cell Research & Therapy. 2018, 9(1):173.
-
under Open Access license CC BY 4.0, without modification.
For Research Use Only. Cannot be used by patients.
Related Services:

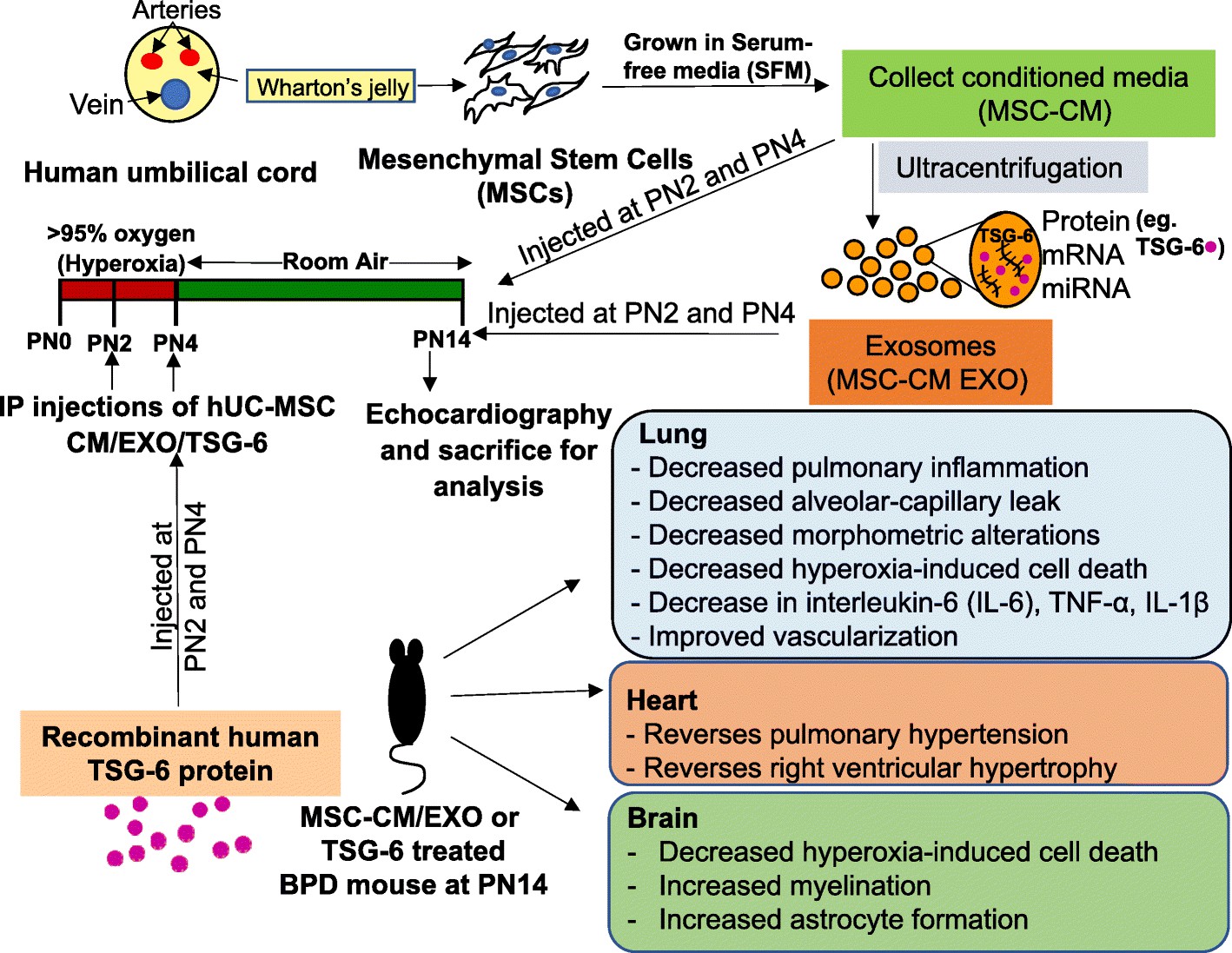 Fig.1 Schematic representation of MSC-CM/EXO/TSG-6 treatment regimen and outcomes in the mouse model of BPD.1,2
Fig.1 Schematic representation of MSC-CM/EXO/TSG-6 treatment regimen and outcomes in the mouse model of BPD.1,2








