Therapeutic Exosomes for Epilepsy
Epilepsy is a chronic neurological disorder of the brain and the fourth leading neurological disorder in the world, affecting the lives of approximately 65 million people. The current antiepileptic drugs are still unable to completely treat epilepsy. A study found that mesenchymal stem cell-derived exosomes (MSC-Exo) can protect the nervous system by reducing neuronal damage caused by seizures. Creative Biolabs has been specializing in exosome research and is committed to providing global customers with high-quality exosome technology to promote the emergence of exosome drugs.
Status Epilepticus (SE)
Epilepsy is a sudden and disabling brain dysfunction that is episodic, transient, repetitive, and stereotyped. Epilepsy is characterized by sudden, abnormal firing of neurons in the brain. Status epilepticus (SE) may lead to neuronal damage and glial hyperplasia. Studies have shown that the occurrence of epilepsy is an extremely complex process involving neurotransmitter signaling, neuronal death, gliosis, synaptic structure, ion channels, and inflammatory responses. The causes of epileptic seizures are also varied. Epilepsy is generally considered to be associated with genetic mutations, neurodegenerative changes, nervous system infections, cerebrovascular disease, and trauma. Studies have confirmed that exosomes and their components are involved in the occurrence and development of epilepsy. Brain neurons and glial cells can secrete exosomes. Moreover, brain injury or stimulation caused by SE can further enhance the secretion of exosomes.
Therapeutic Exosomes for Epilepsy
Acute seizures of epilepsy can be both dangerous and devastating in the lives of people with epilepsy. SE is usually terminated with antiepileptic drug therapy. But SE can lead to hippocampal dysfunction, neurodegeneration, and deficits in cognition and memory. Therefore, there is an urgent need to find an adjunctive therapy to antiepileptic drugs to prevent the development of epilepsy. Several studies have shown that MSC-Exo has a therapeutic effect on neurological diseases, such as Alzheimer's disease, stroke, etc. Intranasal administration (INA) refers to a non-invasive therapy in which drugs are absorbed by the nasal mucosa in the nasal cavity to exert local or systemic therapeutic effects. Due to the proximity of the nasal mucosa to the brain, INA can rapidly reach drug concentrations that treat the brain and spinal cord. Recently, a nasal spray for the treatment of epilepsy has been approved by the FDA (Food and Drug Administration). In addition, the INA of human bone marrow mesenchymal stem cell-derived exosomes (hBMSC-Exo) has been previously demonstrated to have good anti-inflammatory properties.
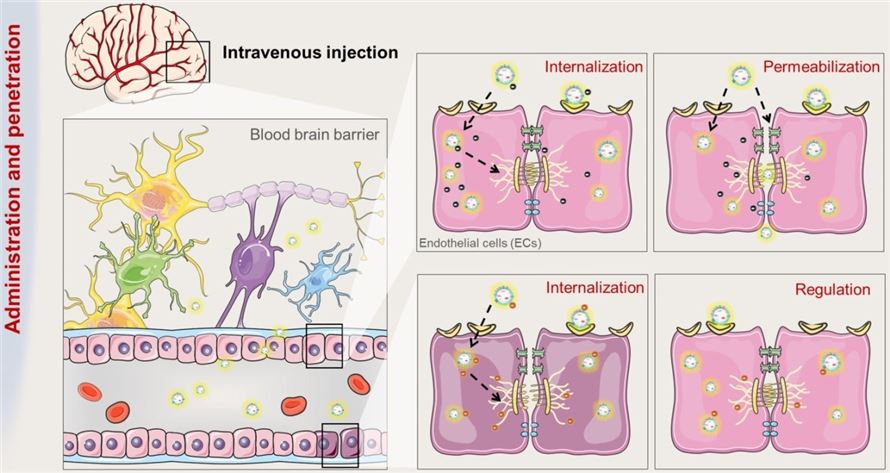 Fig.1 The route and mechanism by which exosomes transport across BBB.1,2
Fig.1 The route and mechanism by which exosomes transport across BBB.1,2
In a mouse model of epilepsy induced by pilocarpine, hBMSC-Exo reached the hippocampus via INA within 6 hours. Epilepsy mice had reduced loss of glutamatergic and GABAergic neurons and greatly reduced inflammation in the hippocampus. Therefore, hBMSC-Exo has a certain protective effect on the nervous system. This study demonstrates that the INA of hBMSC-Exo is effective in reducing the adverse effects of epilepsy in the hippocampus and preventing epilepsy-induced cognitive and memory impairment.
Creative Biolabs has always been concerned about the progress of exosome therapy. You can find anything you need for exosome research here. You are welcome to contact us anytime to discuss your views on epilepsy-related exosomal drugs.
References
-
Xu, M.; et al. Engineered exosomes: desirable target-tracking characteristics for cerebrovascular and neurodegenerative disease therapies. Theranostics. 2021, 11(18):8926-8944.
-
under Open Access license CC BY 4.0, without modification.
For Research Use Only. Cannot be used by patients.
Related Services:

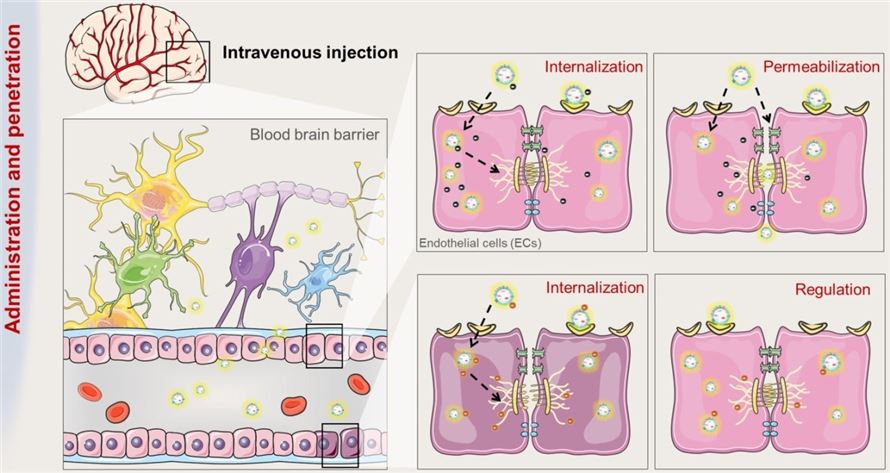 Fig.1 The route and mechanism by which exosomes transport across BBB.1,2
Fig.1 The route and mechanism by which exosomes transport across BBB.1,2








