Therapeutic Exosomes for Non-Small Cell Lung Cancer
Due to their natural structural properties and functions in intercellular communication, exosomes have emerged as drug delivery vehicles for the therapy of non-small cell lung cancer (NSCLC). Creative Biolabs has been committed to the development of exosome carriers and other related technologies to provide customers with therapeutic exosome research services for NSCLC. We introduce the therapeutic application of exosomes in NSCLC, which supports the application prospects of exosome drugs.
Non-small Cell Lung Cancer (NSCLC) and Exosome
Lung cancer remains the largest cause of cancer-related death in both men and women globally, accounting for approximately 27% of all cancer-related deaths. Lung cancer can be divided into two broad categories based on histomorphology: small cell lung cancer (SCLC), which is an aggressive type of lung cancer, and non-small cell lung cancer (NSCLC), which exhibits slower progression. Among them, NSCLC accounts for approximately 85% and is one of the most common malignant tumors. Due to the advanced diagnosis, rapid metastasis, and easy recurrence, only about 15% of NSCLC patients survive for more than 5 years. As mediators of intercellular communication, exosomes act as a "double-edged sword" and have a close link with NSCLC. It can promote the proliferation and spread of NSCLC cells and plays a key role in the occurrence, metastasis, and progression of NSCLC. Meanwhile, exosomes can be used for the diagnosis and treatment of NSCLC. Due to the interesting endogenous functions of exosomes, exosomes are also considered as potential new-generation natural nano drug carriers to transport, protect, and target the delivery of bioactive molecules that alter the function of NSCLC cells.
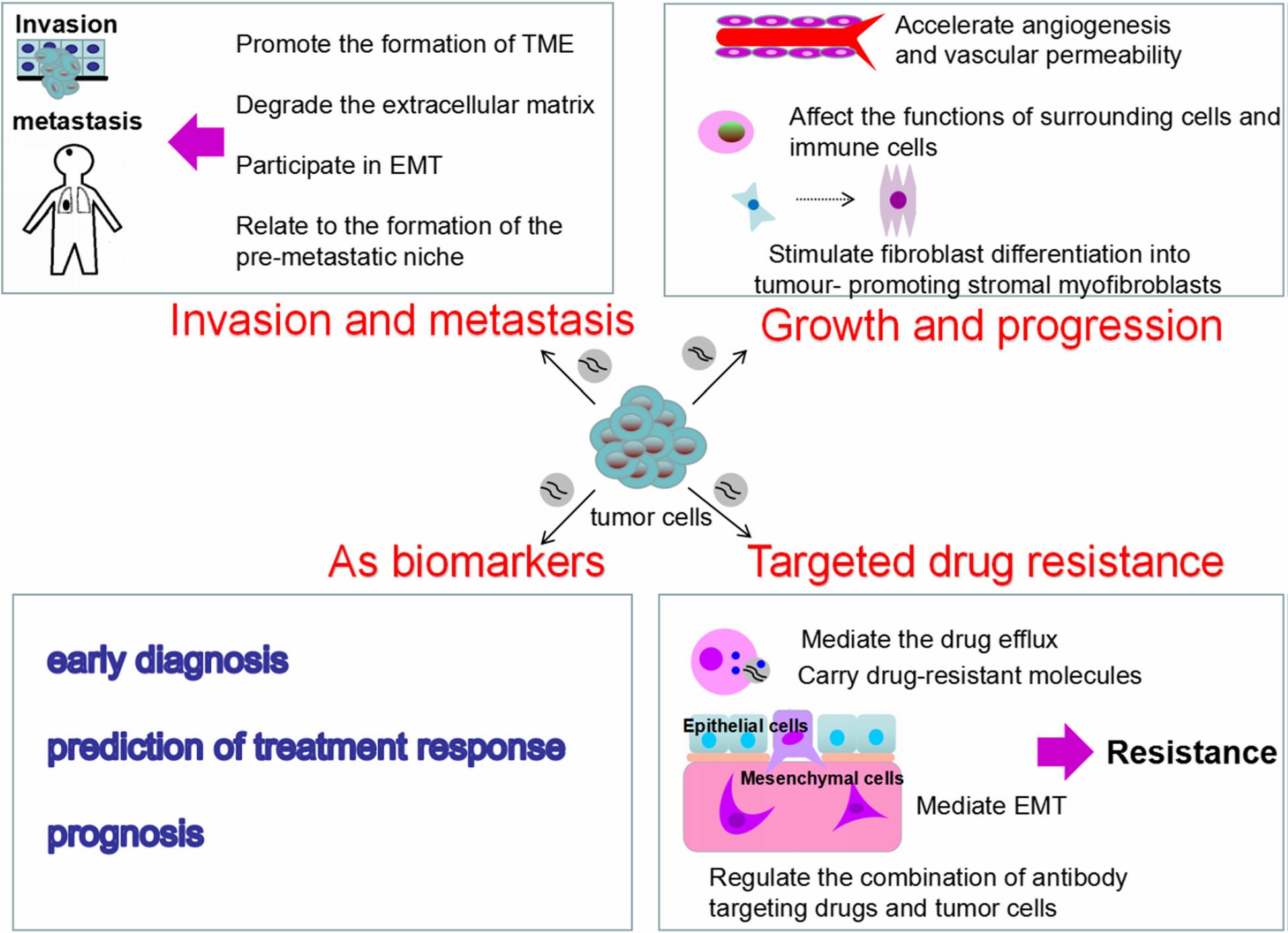 Fig.1 Roles of Tumor-derived exosomes in the NSCLC.1,3
Fig.1 Roles of Tumor-derived exosomes in the NSCLC.1,3
Therapeutic Exosomes for NSCLC
Taxane-based drug Doc*taxe and paclitaxel (PAC) are the first-line antitumor drugs for the treatment of NSCLC. However, clinical treatment is greatly limited due to the low water solubility of these drugs. Compared with the corresponding free drugs, DTX and PAC encapsulated in exosomes significantly inhibited tumor cell proliferation, reduced tumor size, and had higher efficacy.
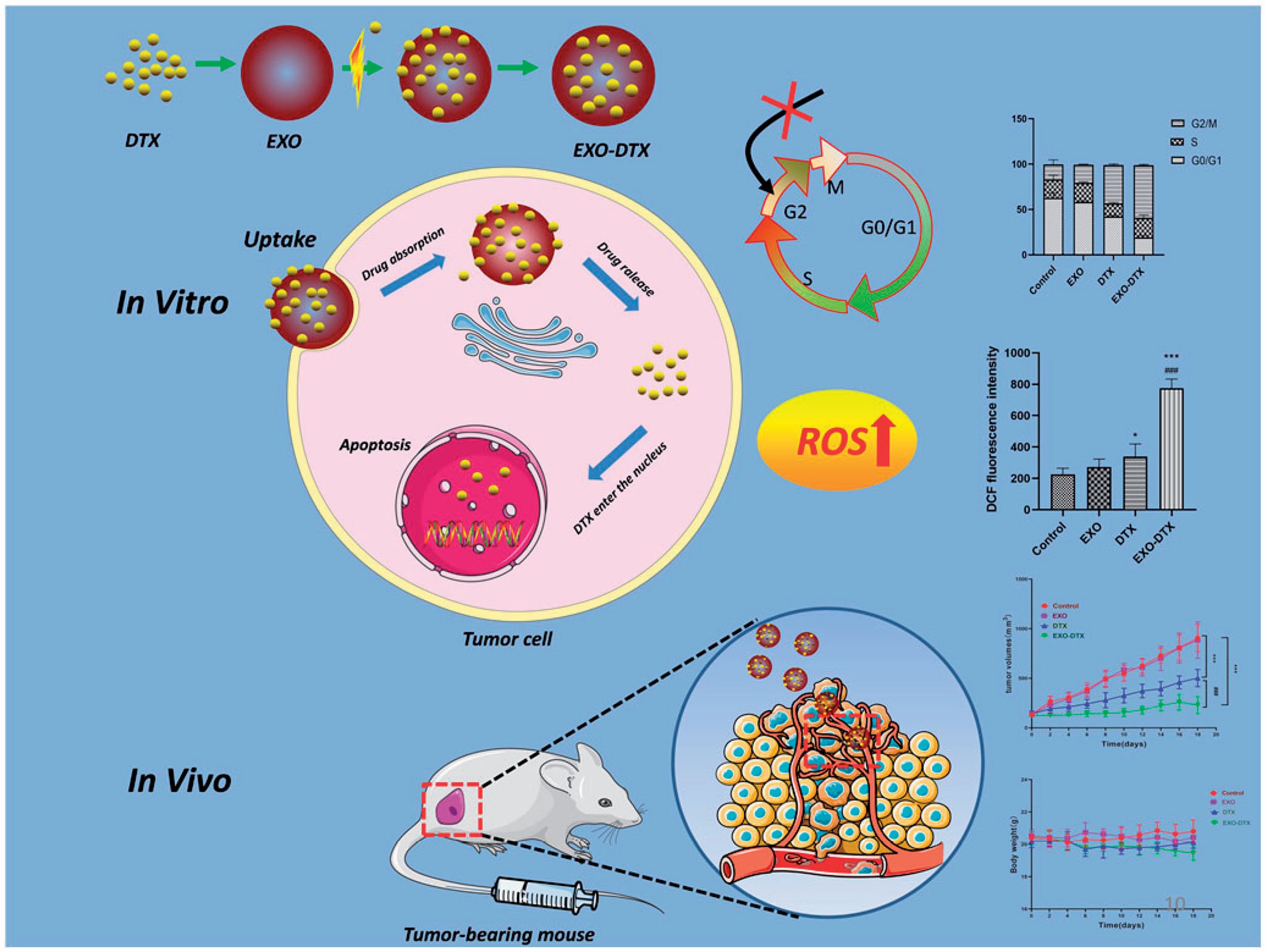 Fig.2 Schematic diagram of the action of EXO-DTX.2,3
Fig.2 Schematic diagram of the action of EXO-DTX.2,3
Immunohistochemistry of human NSCLC tissue has shown that higher levels of C/EBPβ protein are expressed compared to normal lung tissue. siRNA knockdown of C/EBPβ reduces the proliferative capacity of NSCLC cells by delaying the G2/M transition in the cell cycle. Exosome-targeted delivery of siRNA-C/EBPβ has been shown to promote the transformation of tumor-associated macrophages from the M2 immunosuppressive phenotype to M1.
Dendritic cell (DC)-derived exosomes (Dex) can induce a strong anti-tumor adaptive immune response, and can also induce antigen-specific immune tolerance under certain conditions. Therefore, Dex can be used as an anti-tumor vaccine carrier. Furthermore, in advanced unresectable NSCLC, standard treatment relies on platinum-based induction chemotherapy. A team of researchers has developed a Dex drug loaded with metronomic cyclophosphamide (mCTX) and anti-NSCLC antigens. mCTX inhibits T regulatory cell (Treg) function and restores the function of T effector cell and NK cell, and Dex activates innate and adaptive immunity. Phase I trials showed the safety and feasibility of the Dex vaccine but were unable to monitor T cell induction in patients. Second-generation Dex has a higher immunostimulatory capacity and is currently being used in phase II trials.
Creative Biolabs is confident to provide a range of services related to exosome drug development, including exosome extraction and identification, exosome drug loading, and in vitro and in vivo functional validation. If you are interested in our services, please feel free to contact us to discuss your experimental protocol further.
References
-
Zheng, H.; et al. The roles of tumor-derived exosomes in non-small cell lung cancer and their clinical implications. Journal of Experimental & Clinical Cancer Research. 2018, 37(1):226.
-
Wang, Y.; et al. Doc*taxe-loaded exosomes for targeting non-small cell lung cancer: preparation and evaluation in vitro and in vivo. Drug Delivery. 2021, 28(1):1510-1523.
-
under Open Access license CC BY 4.0, without modification.
For Research Use Only. Cannot be used by patients.
Related Services:

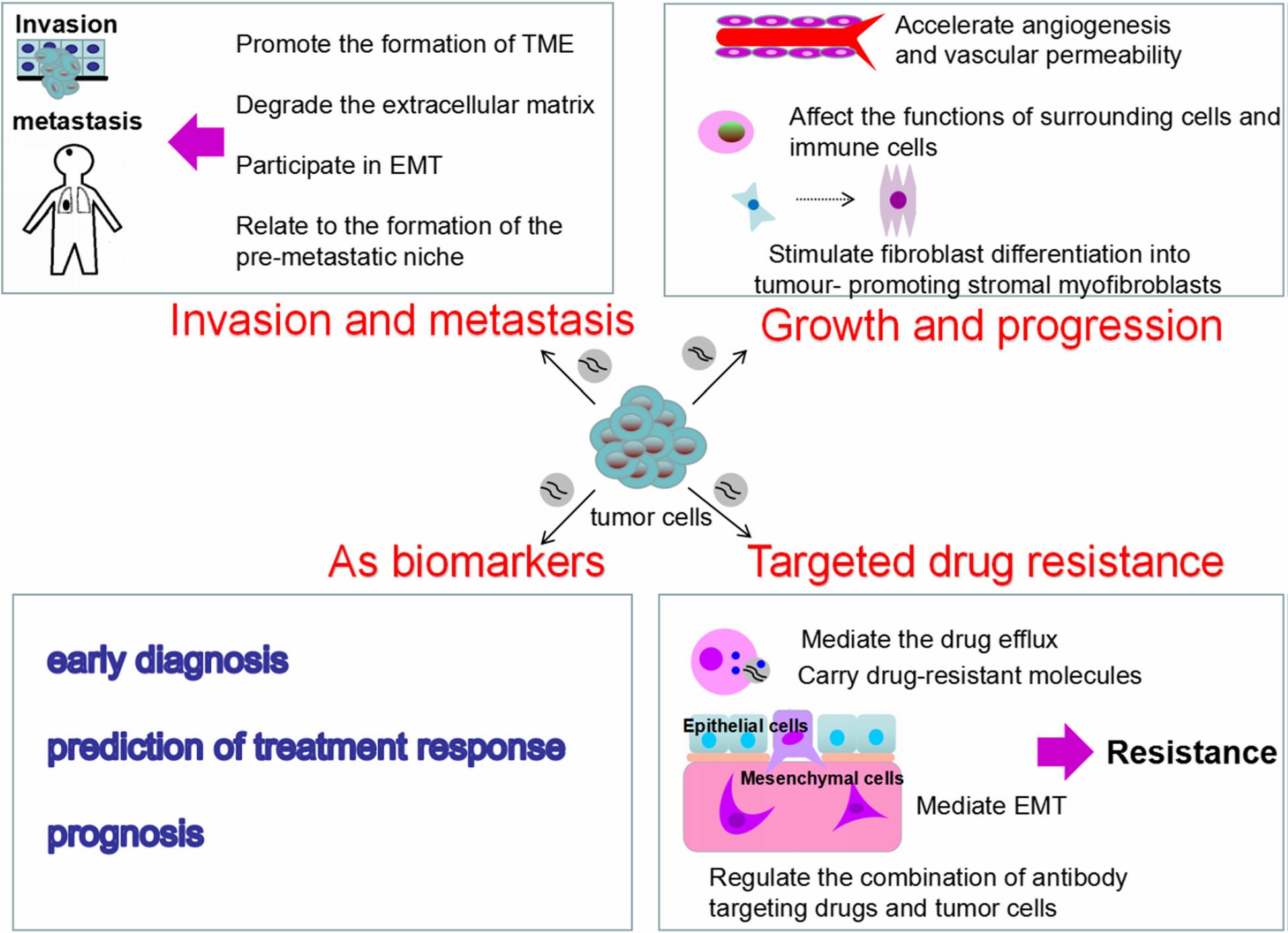 Fig.1 Roles of Tumor-derived exosomes in the NSCLC.1,3
Fig.1 Roles of Tumor-derived exosomes in the NSCLC.1,3
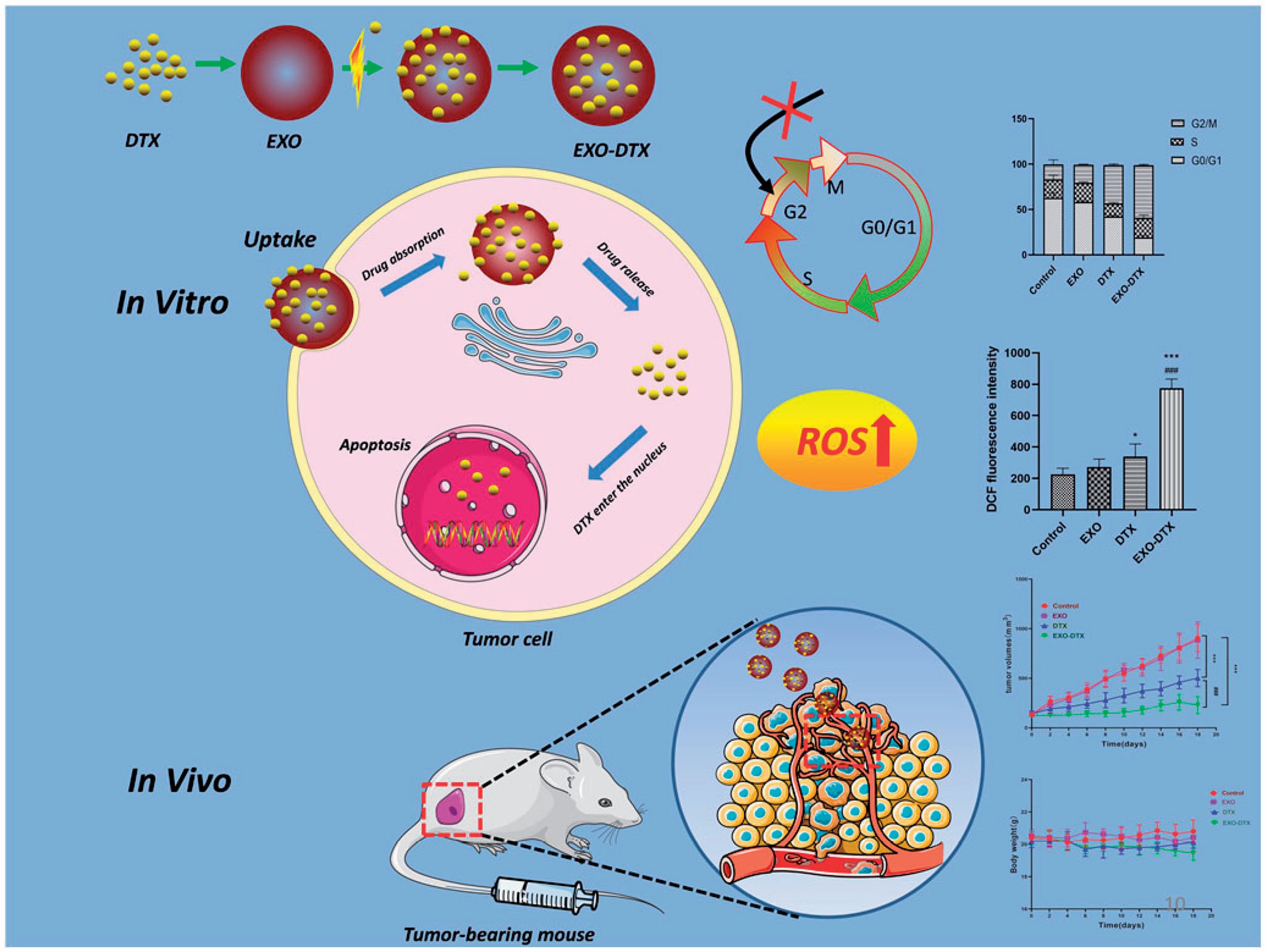 Fig.2 Schematic diagram of the action of EXO-DTX.2,3
Fig.2 Schematic diagram of the action of EXO-DTX.2,3








