Overview Mechanism CDC vs ADCC Assay Protocol Application
Complement-dependent cytotoxicity (CDC) is a crucial immune mechanism that contributes to the elimination of pathogens, tumor cells, and other targets within the body. By utilizing the complement system, CDC operates as a highly effective defense mechanism, enabling the immune system to recognize and destroy cells that are tagged for destruction.
What is Complement-Dependent Cytotoxicity?
CDC is a critical immunological process where the complement system is activated to induce cell death. CDC has become an important mechanism in immunotherapy, especially in the context of monoclonal antibody (mAb)-mediated cytotoxicity.
The Complement System: A Key Player
The complement system consists of a series of small proteins (about 30 in total) found in blood plasma and interstitial fluids. These proteins work in concert to defend the host against infections, clear dead cells, and modulate the immune system.
-
The complement system enhances the recognition and elimination of pathogens by coating them with complement proteins, thus promoting phagocytosis.
-
Complement activation triggers the release of pro-inflammatory molecules that recruit immune cells to the site of infection or injury.
-
In the final stage of activation, the complement proteins form the membrane attack complex (MAC), which disrupts the integrity of pathogen membranes, leading to lysis.
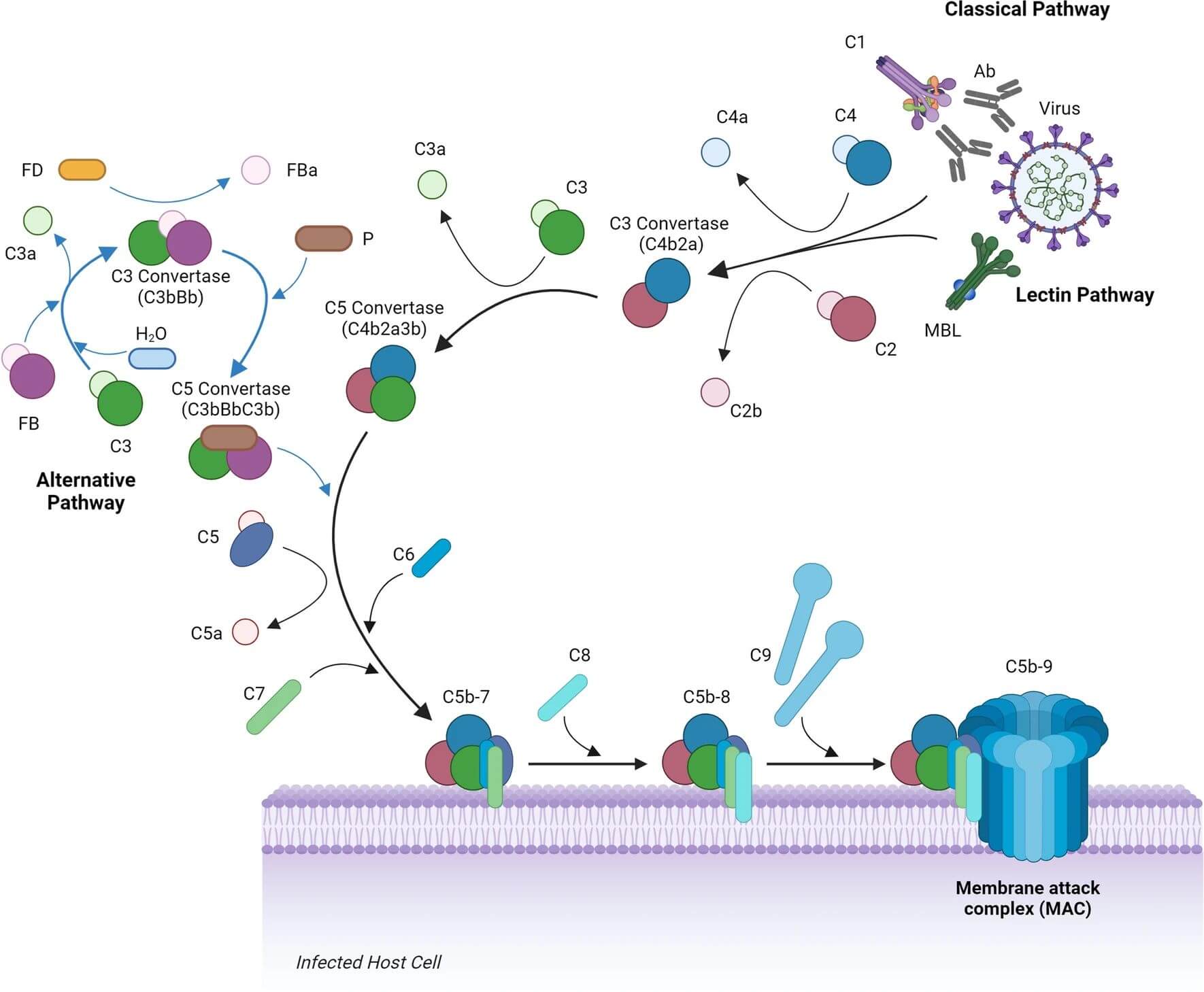
The complement system can be activated through three distinct pathways: the classical pathway, the alternative pathway, and the lectin pathway. Each of these pathways converges on the generation of a key protein, C3b, which initiates the cascade leading to either pathogen destruction or modulation of immune responses.
Complement-Dependent Cytotoxicity
CDC refers to the process by which complement activation leads to the killing of target cells, often cancer cells or infected cells, through the formation of the MAC on the target cell membrane. This immune response is typically triggered when antibodies bind to antigens on the surface of the target cells. These antibodies may be naturally produced or be therapeutic mAbs, both of which can activate the complement system to mediate cell death.
CDC is one of the critical effector functions in antibody-mediated immunity, and understanding this process is vital for developing effective therapeutic strategies that leverage the complement system.
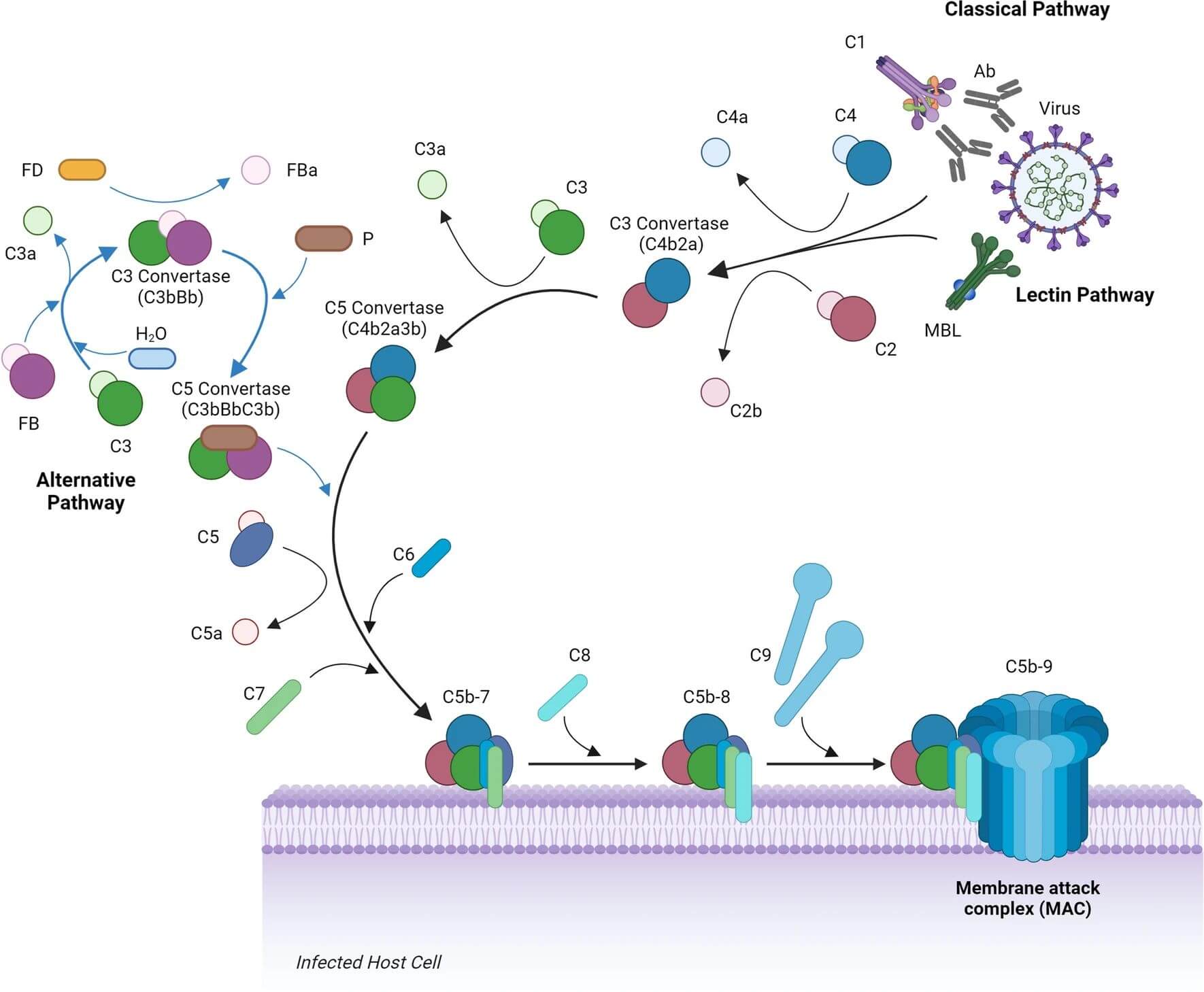
Fig. 1 Overview of the complement system in response to viral infection, demonstrating the classical, lectin, and alternative pathways.1,3
Complement Dependent Cytotoxicity Mechanism
CDC is initiated by the interaction of antigen-specific antibodies with antigens present on the surface of target cells. The process involves the following steps:
Table 1 The steps in CDC.
|
Step
|
Description
|
Key Component
|
|
Antibody Binding
|
CDC begins when an antibody binds to a target antigen on the surface of a cell.
|
-
These antibodies are typically of the IgG or IgM class, with IgG being the most common in CDC.
|
|
Complement Activation
|
The antibody binding activates the classical pathway of the complement system. This initiates a cascade of enzymatic reactions.
|
-
The C1 complex, consisting of C1q, C1r, and C1s, binds to the Fc region of the antibody.
-
The cleavage of complement proteins C4, C2, and finally the activation of C3.
|
|
Formation of C3b
|
The activation of C3 results in the deposition of C3b on the surface of the target cell. C3b serves as an opsonin, facilitating the further activation of complement and the assembly of the MAC.
|
-
C3 is cleaved into C3a and C3b by the complement enzymes.
-
C3b is to facilitate the assembly of the C5 convertase, which leads to MAC formation.
|
|
MAC Formation
|
The MAC is the final effector complex in complement activation, responsible for causing cell lysis.
|
-
The C5 convertase cleaves C5 into C5a and C5b.
-
C5b binds to the target cell membrane and, together with C6, C7, C8, and multiple copies of C9, forms the MAC.
|
|
Cell Death
|
The formation of the MAC results in osmotic imbalance and leakage of essential cellular contents, which causes cell death. This can occur through necrosis or apoptosis, depending on the context and the nature of the target cell.
|
-
The MAC creates a pore in the target cell membrane, leading to ion influx, membrane disruption, and ultimately cell lysis.
|
Types of Cells Targeted by Complement-Dependent Cytotoxicity
-
Tumor Cells: Cancer cells are often targeted by CDC, particularly in the context of monoclonal antibody therapies. mAbs can bind to tumor-specific antigens and trigger CDC.
-
Infected Cells: Cells infected with viruses or other pathogens can also be targeted by the complement system if appropriate antibodies are present.
-
Transplanted Cells: Complement activation can play a role in the rejection of transplanted tissues, where antibodies may bind to antigens on the transplanted cells, initiating CDC.
Factors Influencing Complement-Dependent Cytotoxicity
The efficiency of CDC is influenced by several factors, including:
-
Antibody Isotype
The type of antibody involved in the initial activation of the complement system can significantly affect CDC. IgG is the most effective isotype for CDC, as it binds strongly to the Fc receptors on immune cells and activates the complement system more efficiently compared to IgM.
-
Cell Surface Characteristics
The presence of regulatory proteins on the surface of target cells can modulate complement activation. For example, decay-accelerating factor (DAF) and membrane cofactor protein (MCP) inhibit the formation of the C3 convertase, preventing excessive complement activation on healthy host cells.
-
Complement Regulators
In addition to DAF and MCP, other regulatory proteins, such as protectin (CD59), inhibit the assembly of the MAC. This is a critical mechanism that prevents the complement system from damaging host tissues.
-
Complement Deficiencies
Deficiencies in specific complement components, such as C3, C4, or C9, can result in impaired CDC responses, leaving the host vulnerable to infections or reduced tumor immunity.
Complement Dependent Cytotoxicity vs Antibody-Dependent Cell-Mediated Cytotoxicity
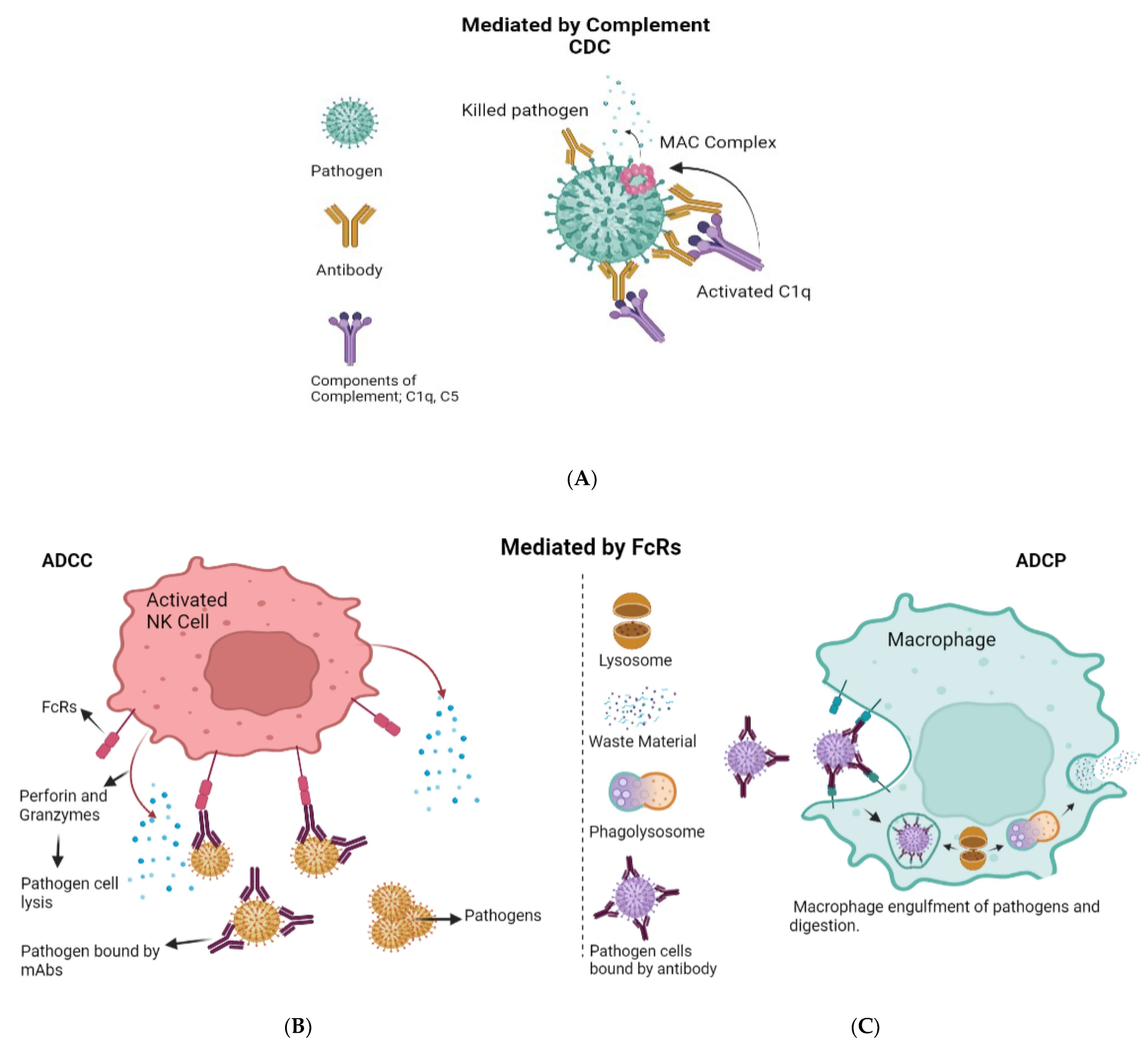
Two key mechanisms of immune-mediated cytotoxicity are CDC and Antibody-Dependent Cell-Mediated Cytotoxicity (ADCC). While both of these processes play pivotal roles in immune responses, they function through distinct mechanisms, leveraging different components of the immune system.
ADCC is a cytotoxic mechanism where immune cells, such as natural killer (NK) cells, macrophages, and neutrophils, are recruited to the site of infection or tumor, where they recognize and kill antibody-coated target cells. Unlike CDC, ADCC does not directly involve complement proteins but instead relies on immune cell receptors that bind to the constant region (Fc region) of antibodies.
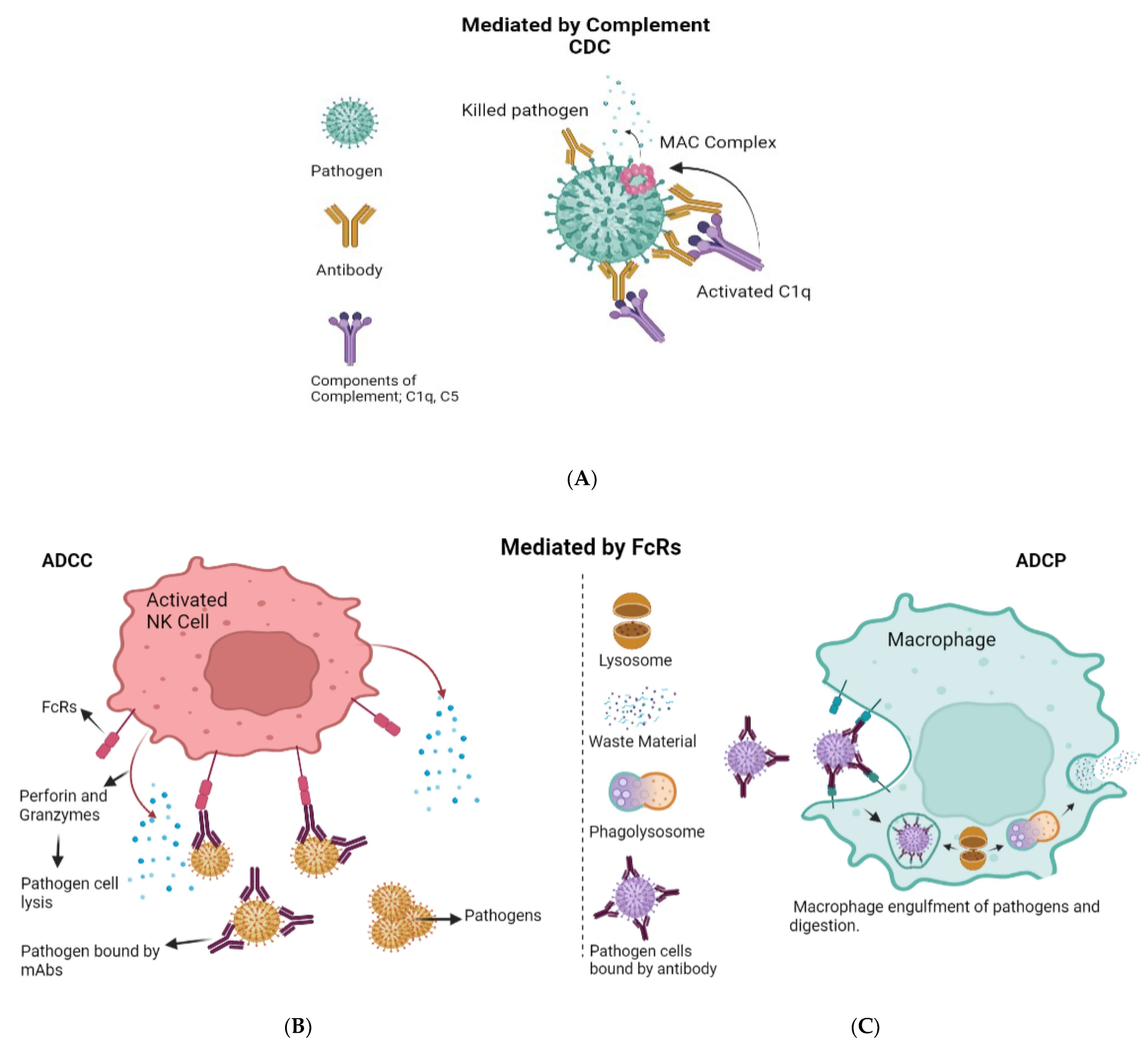
Fig. 2 Antibody effector functions.2,3
Table 2 Key differences between CDC and ADCC.
|
Feature
|
CDC
|
ADCC
|
|
Mechanism
|
Activation of the complement system leading to MAC formation and cell lysis
|
Activation of immune cells, particularly NK cells, to kill target cells via Fcγ receptor binding
|
|
Key Effector Cells
|
Complement proteins (C1q, C3b, C5b, etc.)
|
NK cells, macrophages, neutrophils
|
|
Type of Immunoglobulins Involved
|
IgG, IgM (primarily IgM in early responses)
|
IgG (most commonly used in therapeutic applications)
|
|
Target Cell Killing
|
Direct lysis by the MAC
|
Cytotoxic molecules released by effector cells
|
|
Efficiency
|
Dependent on complement availability and target antigen expression
|
Dependent on immune cell activity and Fc receptor engagement
|
|
Therapeutic Relevance
|
Commonly targeted in autoimmune and cancer therapies
|
Central to the action of many monoclonal mAb-based therapies
|
Complement Dependent Cytotoxicity Assay
The complement dependent cytotoxicity test measures the ability of antibodies to mediate complement activation and target cell lysis. There are several components and methodological steps involved in performing a CDC assay, including selecting appropriate cellular models, antibodies, and complement sources, as well as choosing suitable readout methods for assessing cell viability.
-
Antibody Selection and Targeting: Monoclonal antibodies are often used due to their specificity for a single epitope on the target antigen. Additionally, antibodies can be engineered to enhance their CDC activity by modifying their Fc regions to improve complement activation.
-
Complement Source: The complement system can be sourced from human or animal serum, depending on the species of the target cells. In many cases, human complement serum is preferred. The serum should be titrated to determine the optimal concentration for the assay.
-
Readout Methods: The readout methods in a CDC assay are used to measure cell viability or cytotoxicity following complement activation. Several approaches can be employed, including:
-
Lactate dehydrogenase (LDH) release assay
-
Flow cytometry
-
Chromium release assay
-
MTT assay
Complement Dependent Cytotoxicity Protocol
To perform a CDC assay, the following reagents and materials are necessary:
-
Target Cells: These may be cancer cell lines, infected cells, or engineered cells expressing specific antigens of interest.
-
Antibodies: Monoclonal antibodies or polyclonal antibodies that specifically bind to antigens on the target cells. Typically, IgG antibodies are used for their effective interaction with the Fc portion of complement proteins.
-
Complement Source: The complement proteins can be obtained from human or animal serum. For a more controlled experiment, purified complement proteins (e.g., C1q, C3, and C5) can be used.
-
Assay Medium: RPMI-1640 or DMEM (depending on the target cell line) supplemented with fetal bovine serum (FBS).
-
Cytotoxicity Detection Kit: A kit such as LDH release assay or MTT assay to assess cell viability and cytotoxicity after treatment.
Table 3 The protocol steps of CDC assay.
|
Steps
|
Specific operations
|
|
Preparation of Target Cells
|
-
Cultivate target cells in appropriate growth media
-
Detach cells using trypsin-EDTA and wash twice with PBS
-
Resuspend cells in assay medium
|
|
Antibody Binding
|
-
Incubate the target cells with a specific concentration of antibody
-
Ensure that the antibody binds to the antigen on the surface of the target cells.
|
|
Complement Addition
|
-
After antibody incubation, add human or animal serum as the source of complement
|
|
Cytotoxicity Detection
|
-
After the incubation period, assess cell viability using an appropriate cytotoxicity assay
|
|
Data Analysis
|
-
Calculate the percentage of cytotoxicity based on the formula
|
Several factors can influence the outcome of CDC assays and should be optimized for accurate and reproducible results.
-
Antibody concentration
-
Complement source
-
Incubation conditions
-
Target cell type
If low cytotoxicity is observed, check for insufficient antibody binding, low complement activity, or improper target cell density. Increasing the antibody concentration or using a different complement source may help.
Application Areas for CDC Bioassays
In the context of immunotherapy, particularly mAb-based therapies, CDC is an essential mechanism through which the therapeutic antibodies exert their anti-tumor or anti-pathogen effects. By enhancing the recruitment and activation of the complement system, mAbs can trigger CDC against malignant cells or pathogenic microbes, thereby boosting the therapeutic effect.
Incorporating CDC testing in the development of complement therapeutics is pivotal for optimizing therapeutic antibodies. By evaluating the ability of monoclonal antibodies or biologic agents to activate the complement cascade, CDC bioassays provide a reliable measure of their efficacy. CDC testing can be used to assess:
-
The potency of therapeutic antibodies in terms of their ability to activate the complement system and induce cell lysis.
-
Target specificity of the antibody, ensuring that complement activation is directed toward the diseased or infected cells.
-
Immune evasion by pathogens or tumor cells, as some cells may downregulate complement activation or upregulate complement inhibitors.
The data obtained from CDC bioassays are essential for optimizing the design of biologics to maximize their therapeutic potential while minimizing off-target effects. From cancer immunotherapy to autoimmune diseases, infectious diseases, and gene therapy, CDC bioassays play a pivotal role in ensuring the success of complement-based therapies.
As our understanding of the complement system grows, the incorporation of CDC testing will remain an integral component in the development of innovative therapies that harness the full potential of the immune system. By continuing to explore new applications and optimizing CDC testing protocols, we can pave the way for more effective and targeted therapeutic interventions.
Creative Biolabs offers a full range of complement-related services and products, including:
If you want more information, please feel free to contact us.
References
-
Mellors, Jack, and Miles Carroll. "Direct enhancement of viral neutralising antibody potency by the complement system: a largely forgotten phenomenon." Cellular and Molecular Life Sciences 81.1 (2024): 22.
-
Mokhtary, Pardis, et al. "Recent progress in the discovery and development of monoclonal antibodies against viral infections." Biomedicines 10.8 (2022): 1861.
-
under Open Access license CC BY 4.0, without modification.
For Research Use Only.
Related Sections: